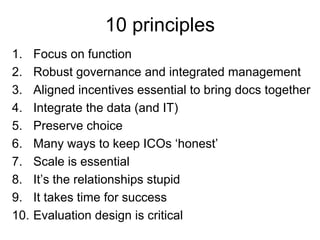
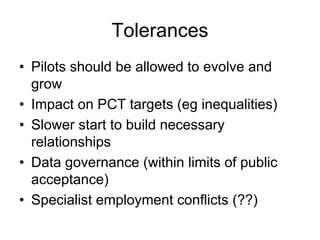
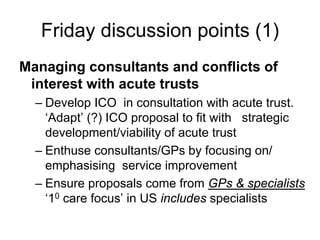
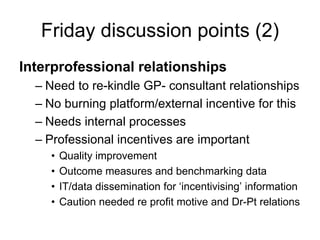
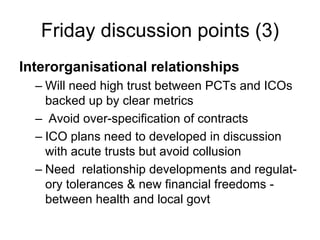
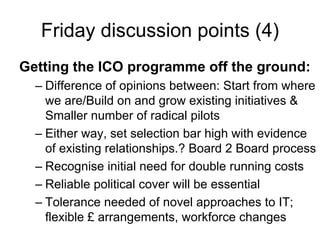
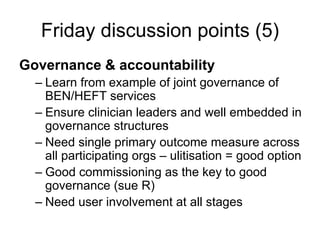
1. The document outlines 10 principles for integrated care organizations (ICOs) and discusses various considerations for establishing ICO pilots, including allowing pilots time to evolve, managing consultant and acute trust relationships, and developing interorganizational relationships between groups.
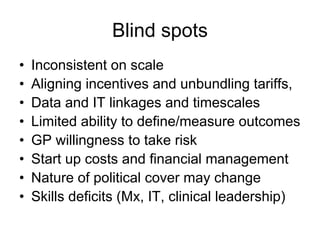
2. It identifies potential blind spots such as inconsistent views on scale, skills deficits, and the changing nature of political support.
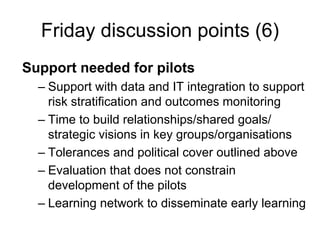
3. The Friday discussion points focus on governance, accountability, and support needs for successful ICO pilots, including relationship-building, data integration, and flexibility.