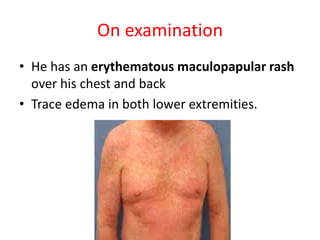
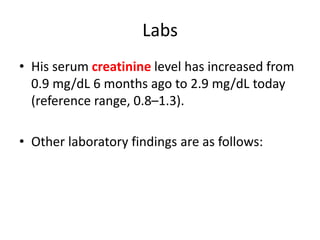
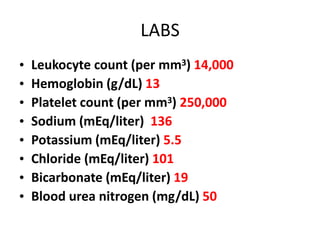
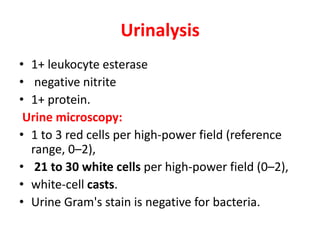
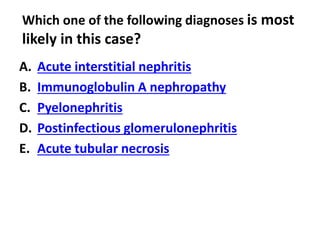
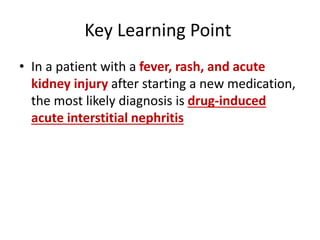
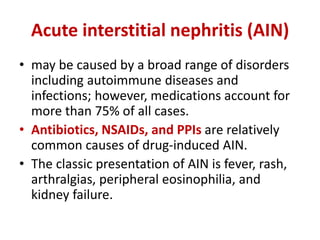
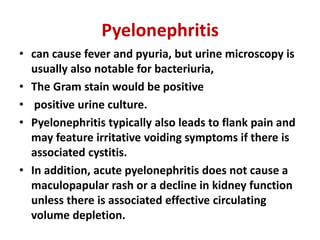
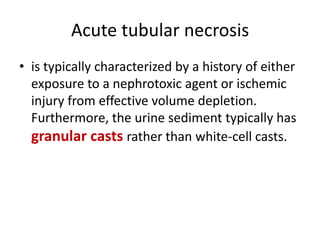
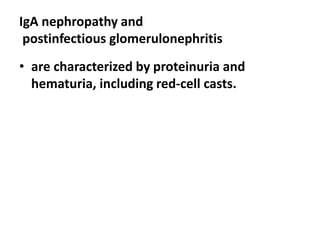
A 40-year-old man presented with nausea, fever, and joint pain, and was found to have acute kidney injury. He had recently been treated for H. pylori infection with omeprazole, amoxicillin, and clarithromycin. On examination, he had a rash and lower extremity edema. Urinalysis showed white blood cells and white cell casts. The diagnosis was acute interstitial nephritis, likely caused by a drug reaction to antibiotics and omeprazole, given the presentation of fever, rash and acute kidney injury after starting new medications.