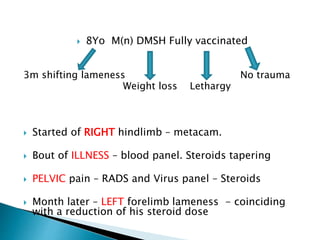
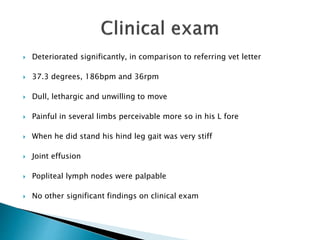
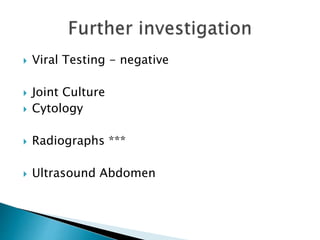
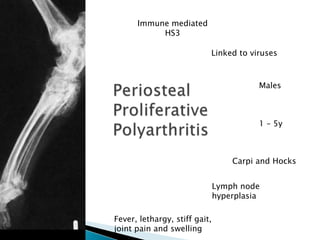
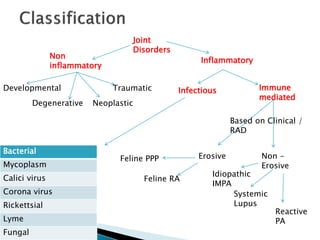
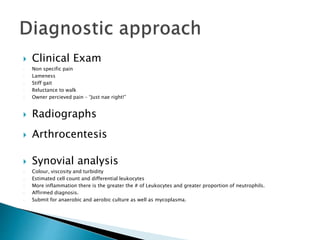
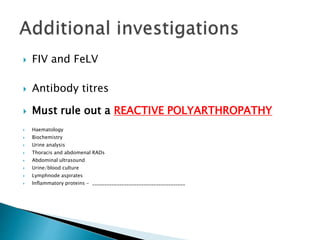
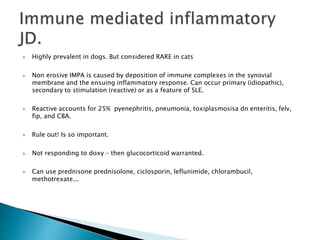
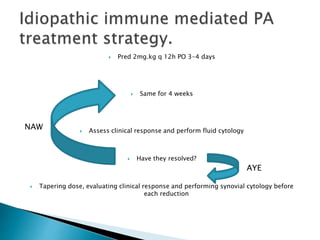
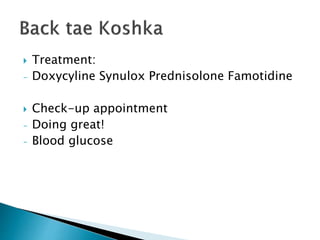
The document outlines the medical history and treatment of an 8-year-old cat experiencing shifting lameness, weight loss, and lethargy, along with a series of diagnostic tests including blood panels, radiographs, and virus testing. The findings suggest conditions related to immune-mediated polyarthritis and other joint disorders, with treatment including steroids and antibiotics. The importance of ruling out infectious and reactive causes, along with careful monitoring and adjustment of treatment based on clinical response, is emphasized.