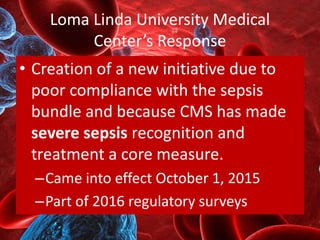
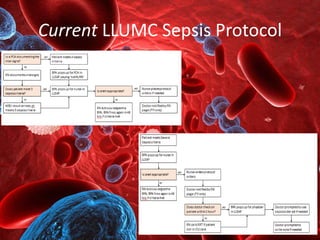
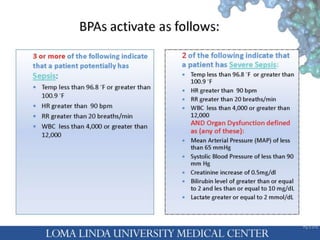
Loma Linda University Medical Center implemented a new initiative to improve sepsis recognition and treatment due to poor compliance with sepsis protocols, effective October 2015. The initiative utilized electronic medical records and alert systems, resulting in faster identification and treatment of sepsis, which decreased hospital mortality and improved discharge rates. Challenges, such as alert fatigue and the need for ongoing staff training, were also noted to ensure compliance and enhance patient outcomes.



![References
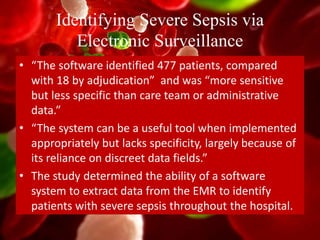
Identifying Severe Sepsis via Electronic Surveillance.
(2015). American Journal of Medical Quality, 30(6),
559-565 7p. doi:10.1177/1062860614541291
Kurczewski, L., Sweet, M., McKnight, R., & Halbritter, K. (2015).
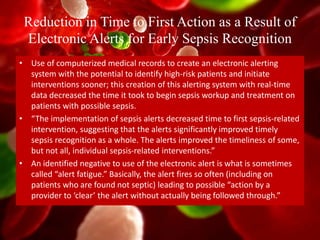
Reduction in Time to First Action as a Result of Electronic
Alerts for Early Sepsis Recognition. Critical Care Nursing
Quarterly, 38(2), 182. doi:10.1097/CNQ.0000000000000060
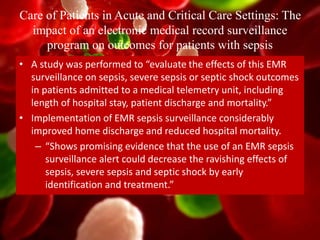
McRee L, Thanavaro J, Moore K, Goldsmith M, Pasvogel A. Care of
Patients in Acute and Critical Care Settings: The impact of an
electronic medical record surveillance program on outcomes
for patients with sepsis. Heart & Lung - The Journal Of Acute
And Critical Care [serial online]. November 1, 2014;43:546-
549. Available from: ScienceDirect, Ipswich, MA. Accessed
November 20, 2015.](https://image.slidesharecdn.com/qualityimprovement-sepsisleadership-151209192559-lva1-app6892/85/Quality-Improvement-Sepsis-Recognition-Treatment-18-320.jpg)