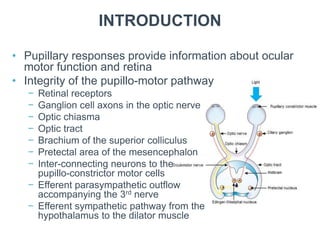
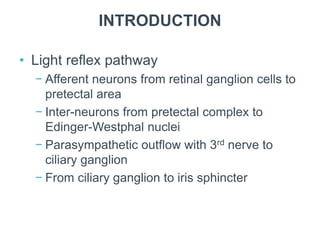
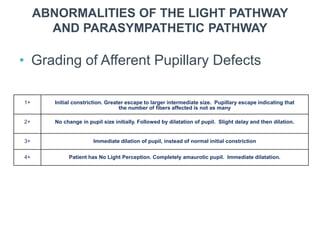
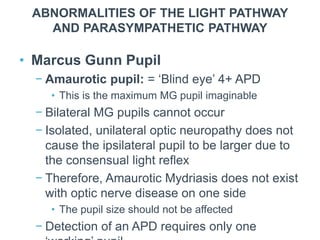
The document discusses various common eye disorders related to pupil functionality and associated neurological conditions. It covers the anatomy and pathways involved in pupillary responses, normal and abnormal pupillary phenomena, and specific conditions such as Marcus Gunn pupil, Argyll Robertson pupil, and Horner syndrome. Pupillary testing methods and their significance in diagnosing underlying neurological issues are also elaborated.