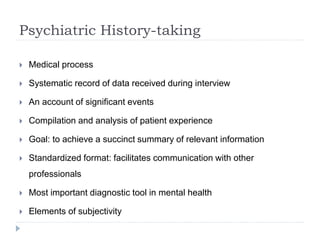
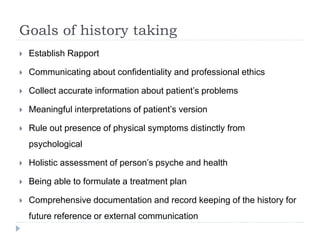
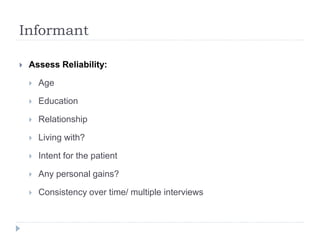
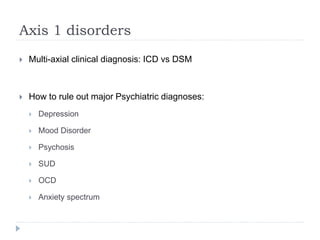
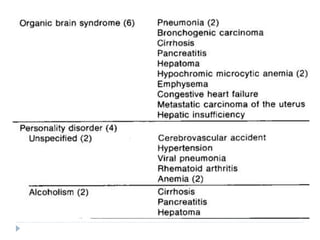
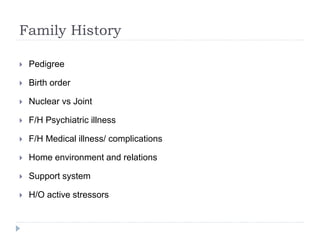
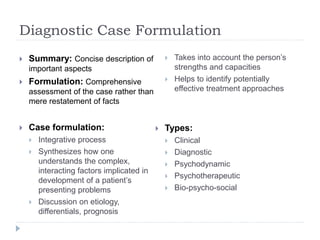
The document outlines the importance of psychiatric history-taking as a systematic process for gathering relevant patient information, emphasizing its role as a primary diagnostic tool in mental health. It details the essential components involved in this procedure, including establishing rapport, gathering demographic information, presenting complaints, and considering family and childhood histories. The summary also highlights the necessity of a holistic assessment that guides treatment planning and interventions, factoring in both psychological and physical health parameters.