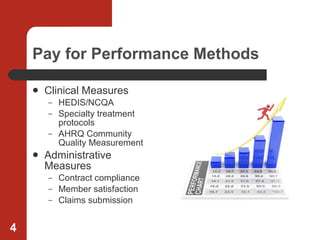
The document discusses strategies for aligning providers with payers through business partnerships, shared savings programs, and loyalty programs. It recommends establishing mutual goals and accountability, clearly communicating policies and performance measures, and rewarding providers for meeting clinical and administrative targets. Loyalty programs should build long-term relationships through referrals, co-marketing, education, and regular communication using various channels.