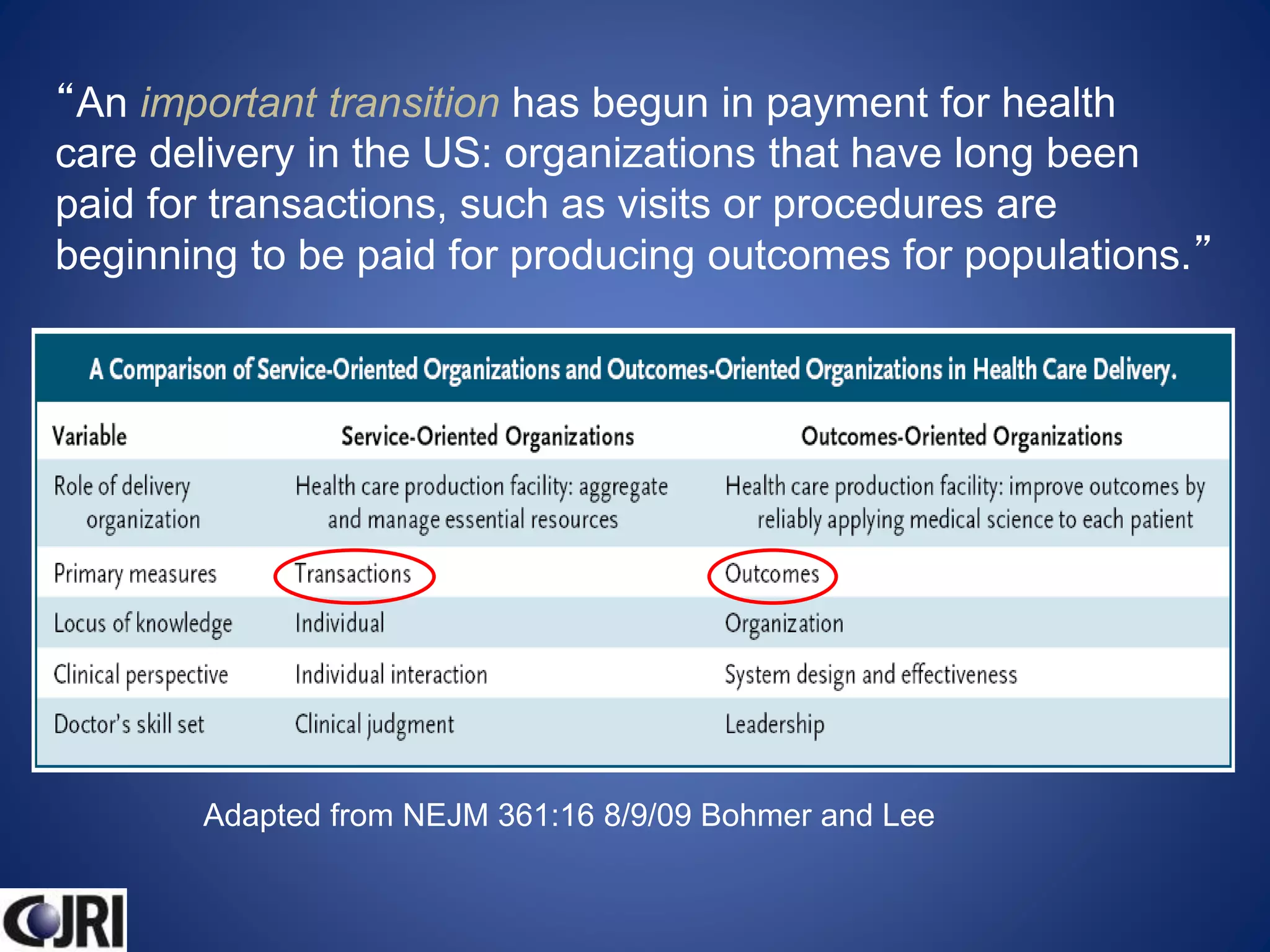
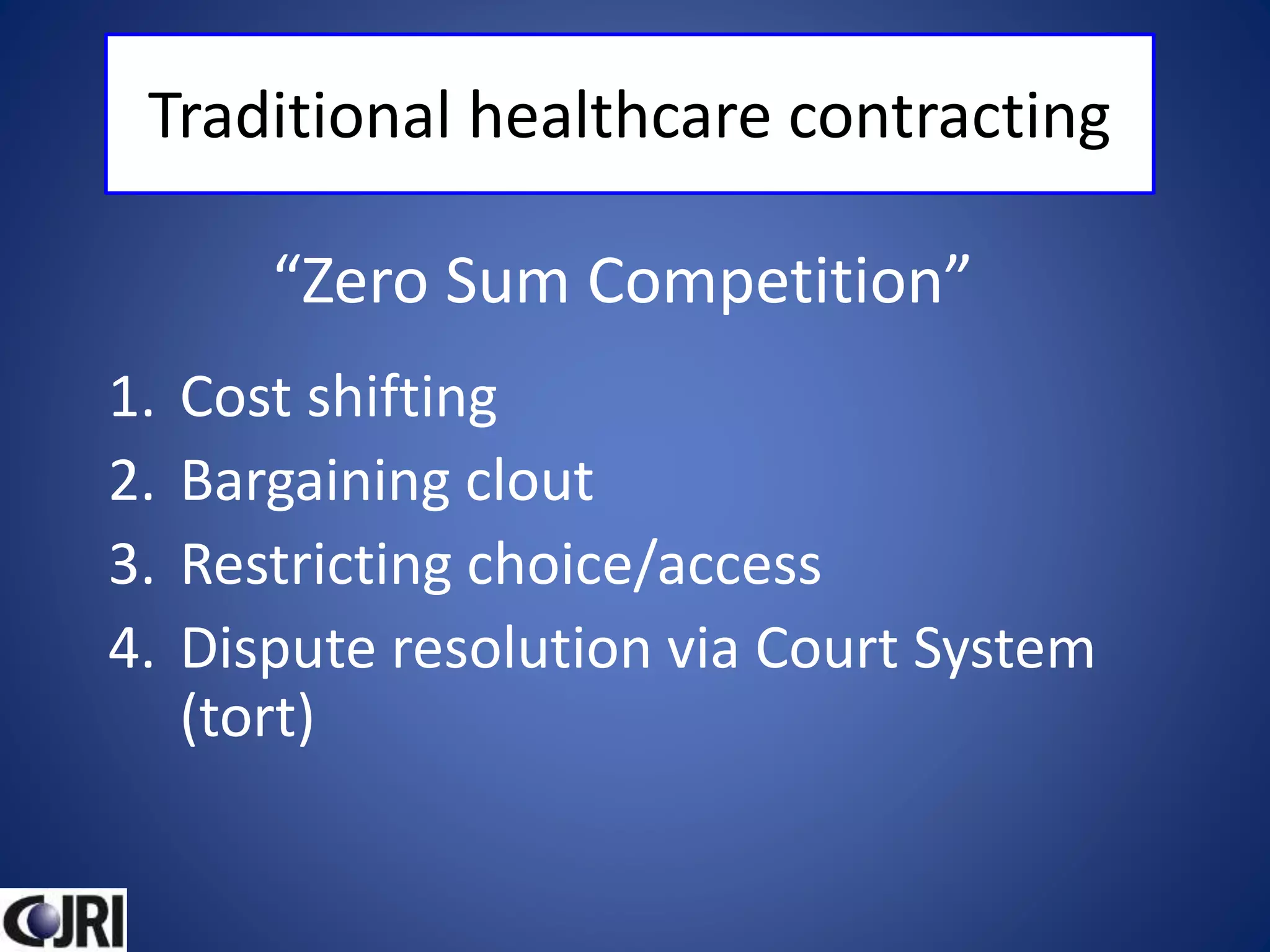
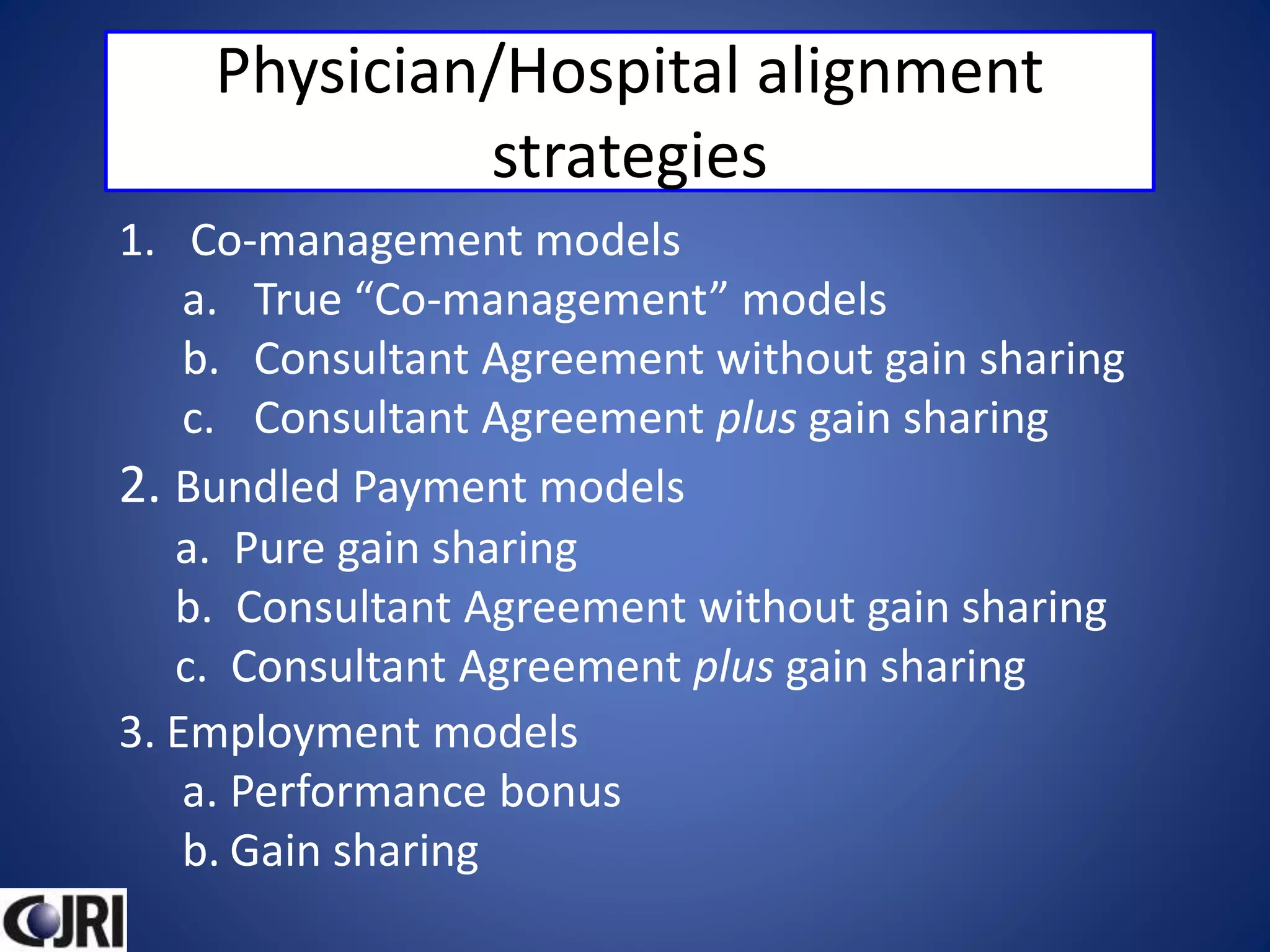
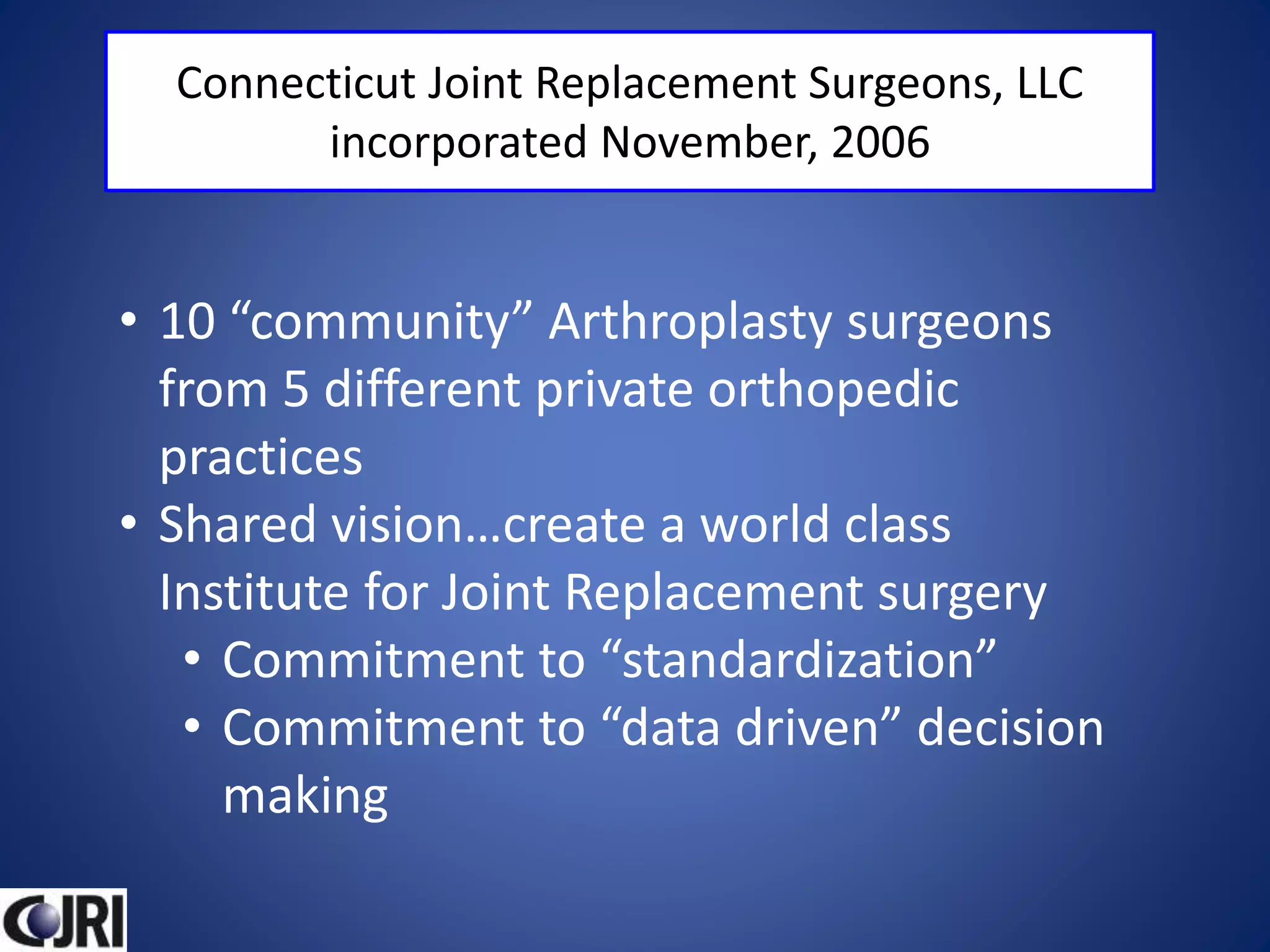
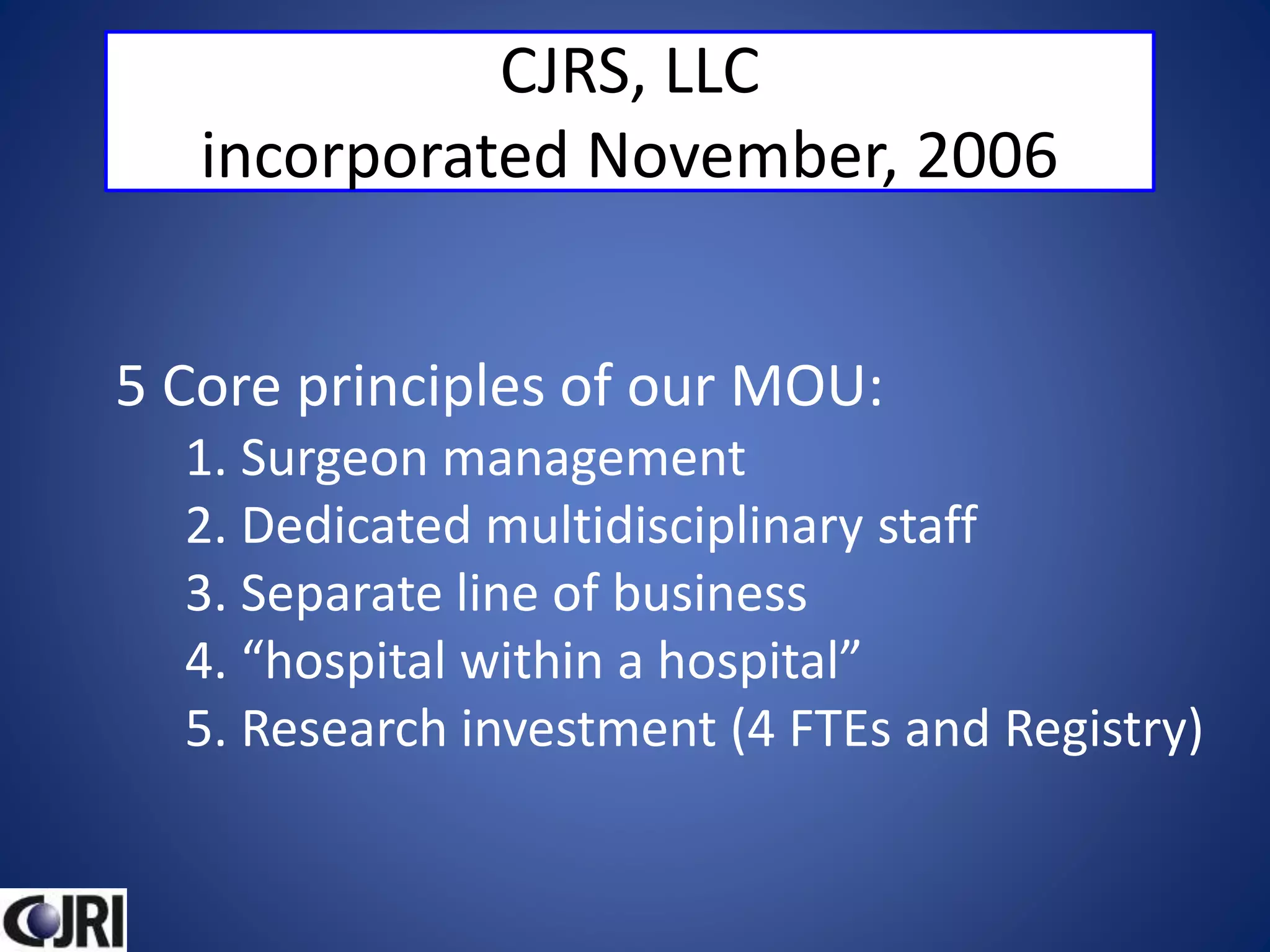
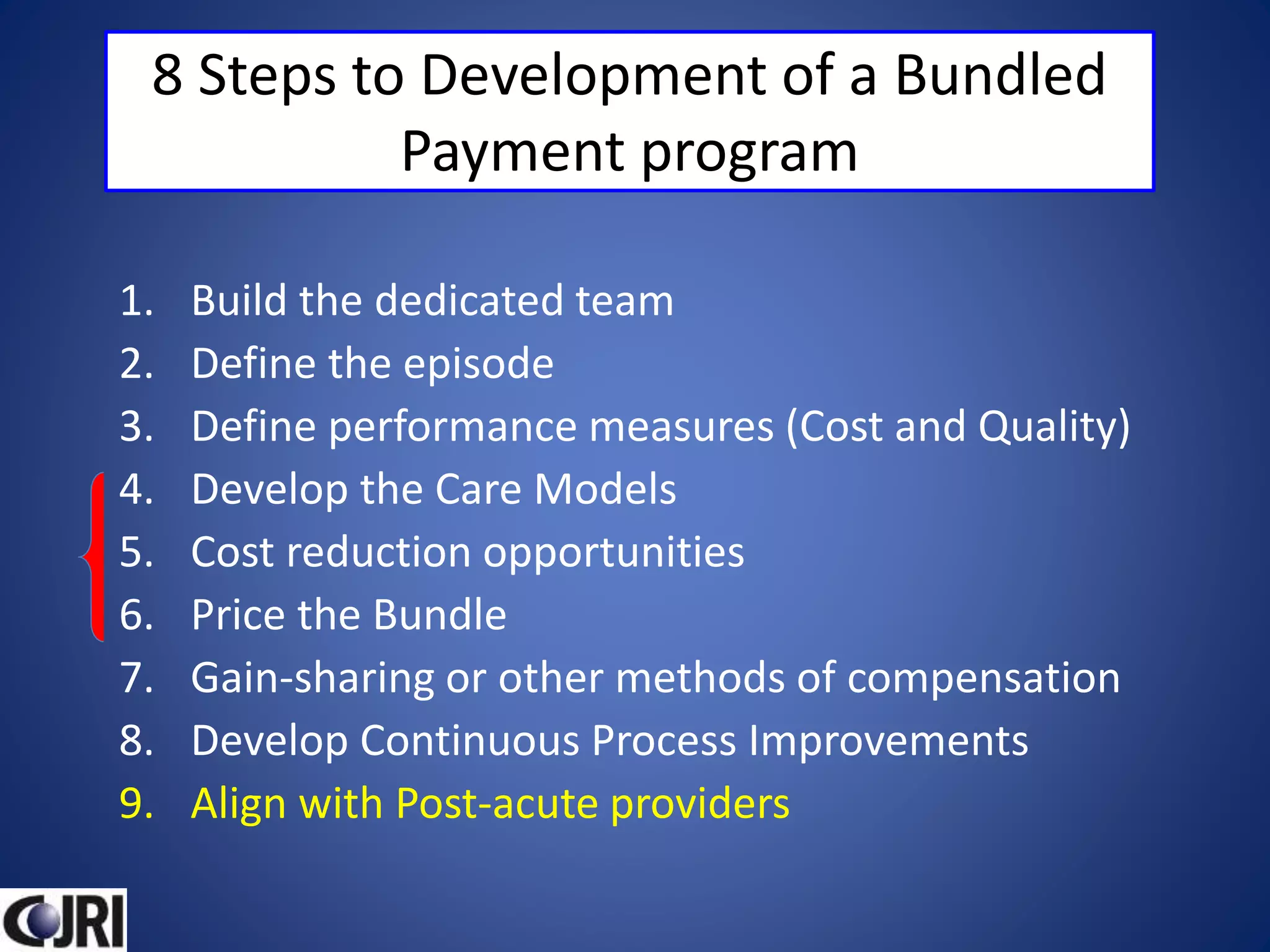
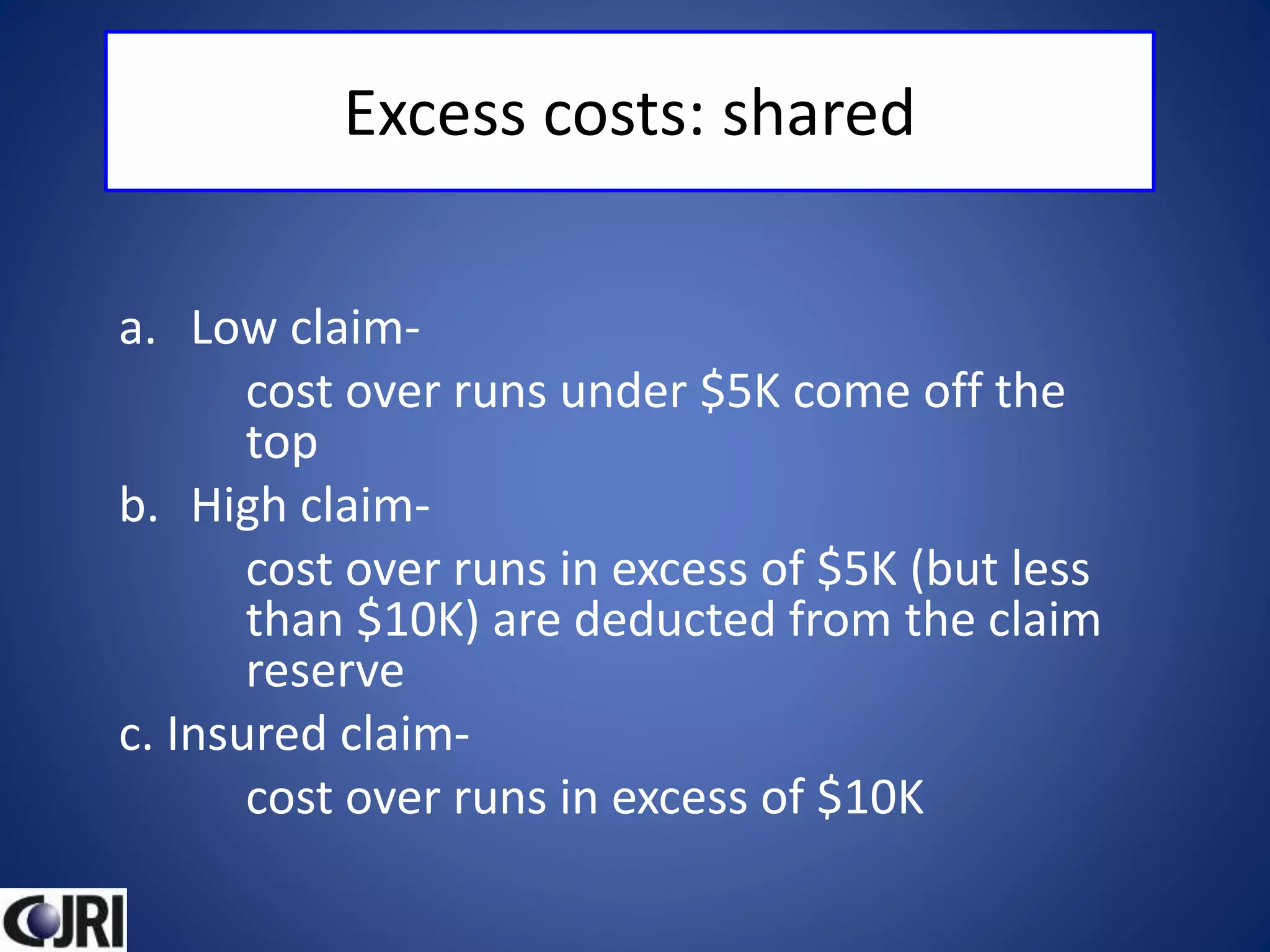
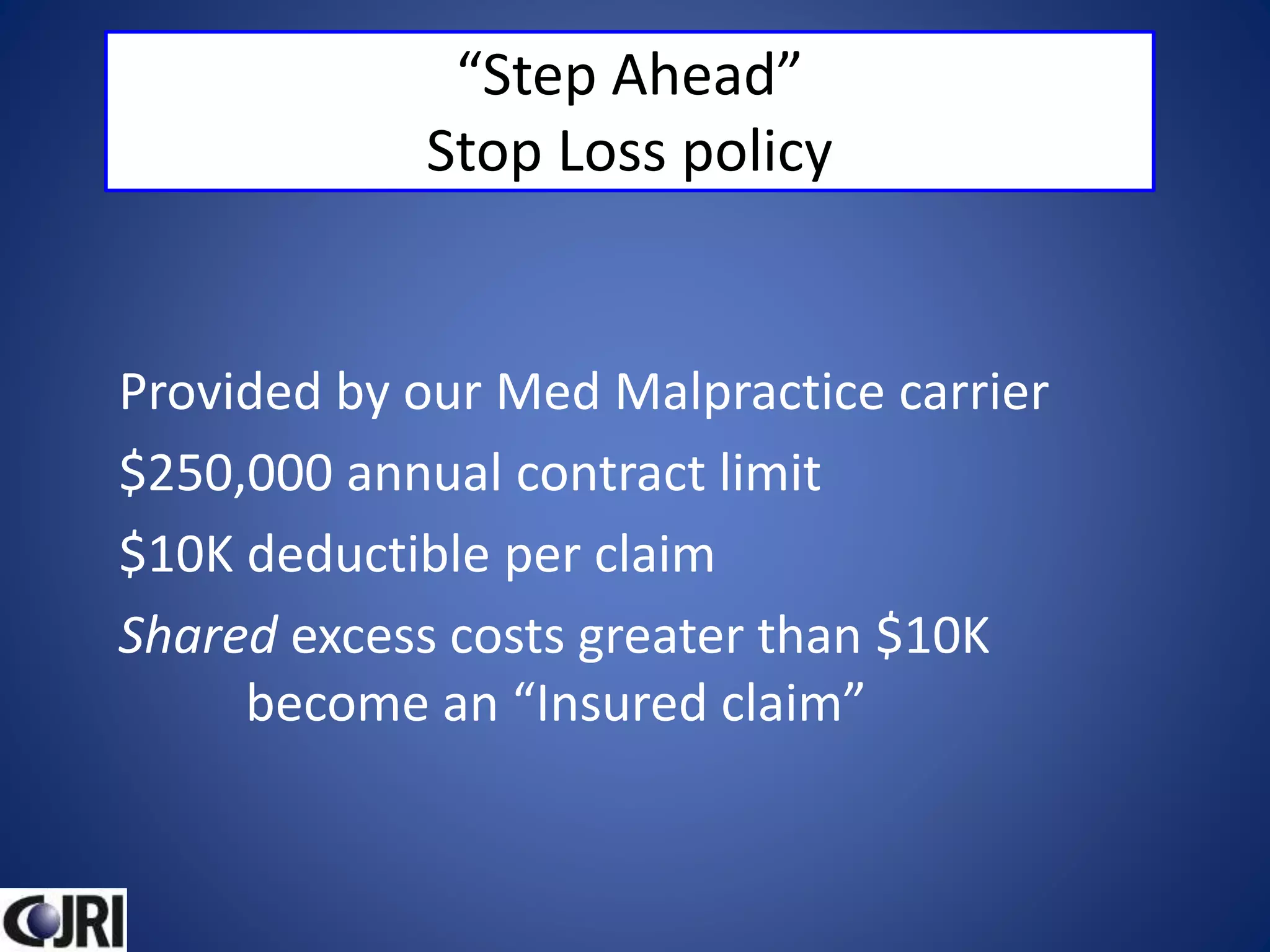
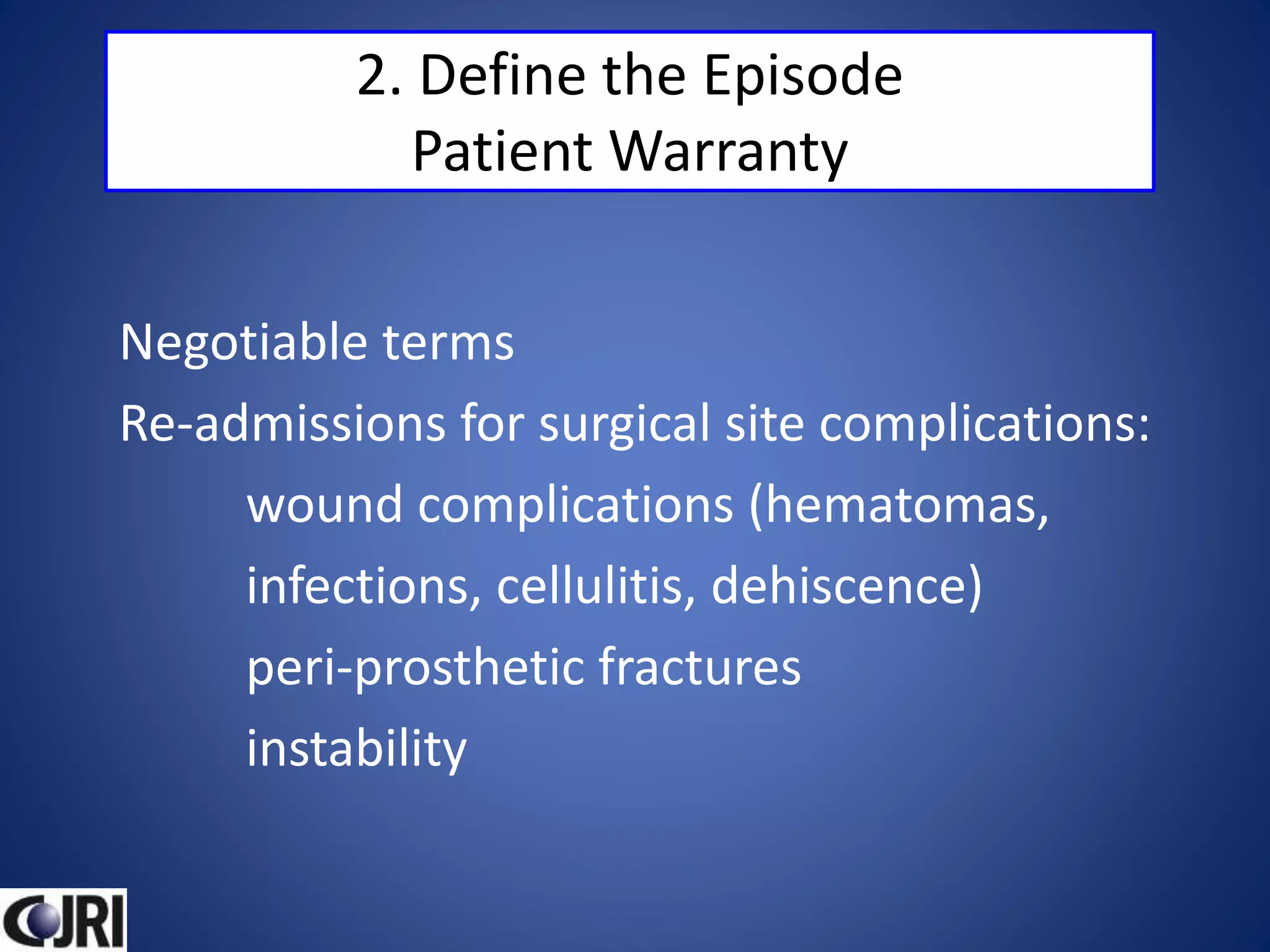
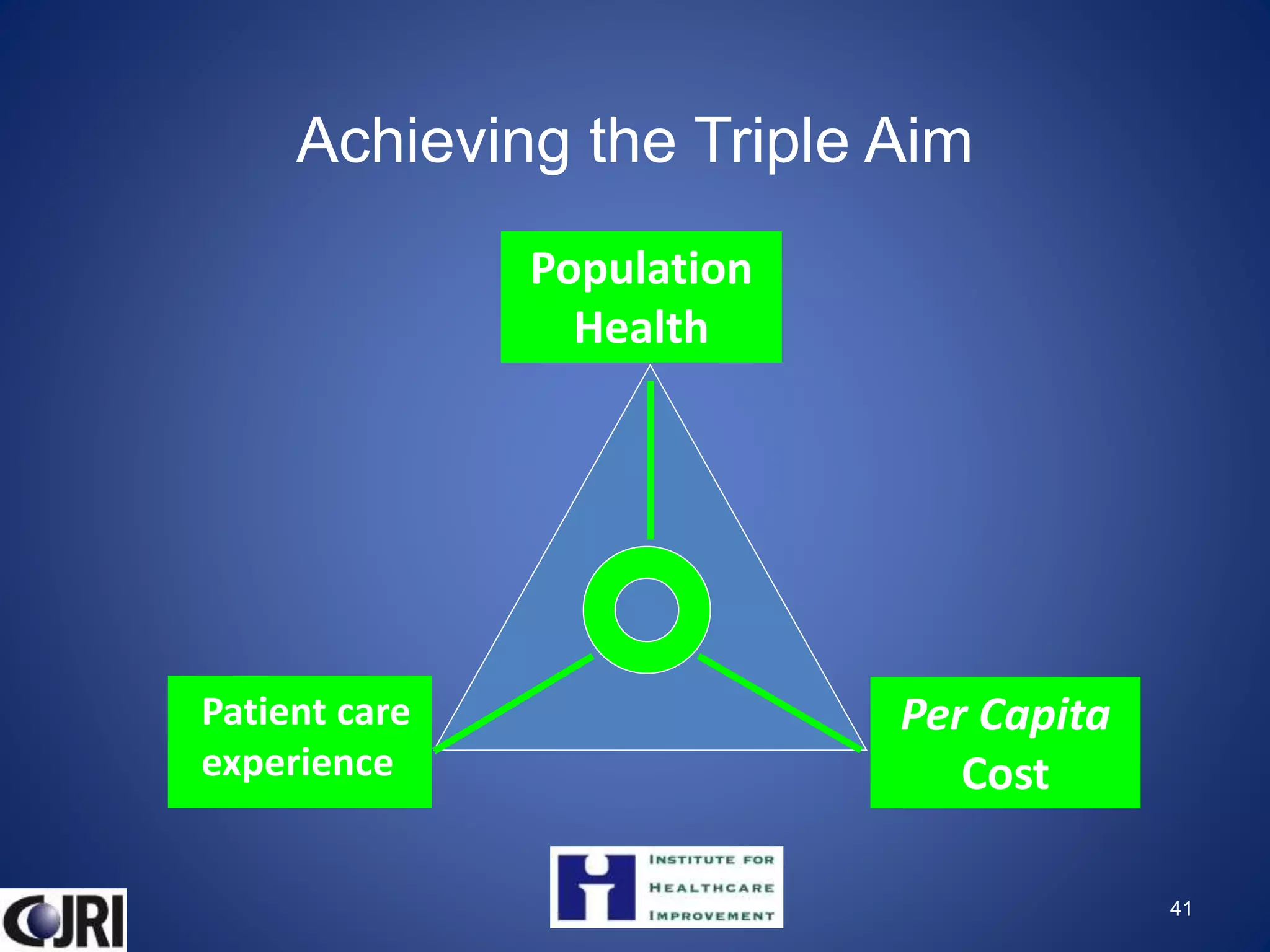
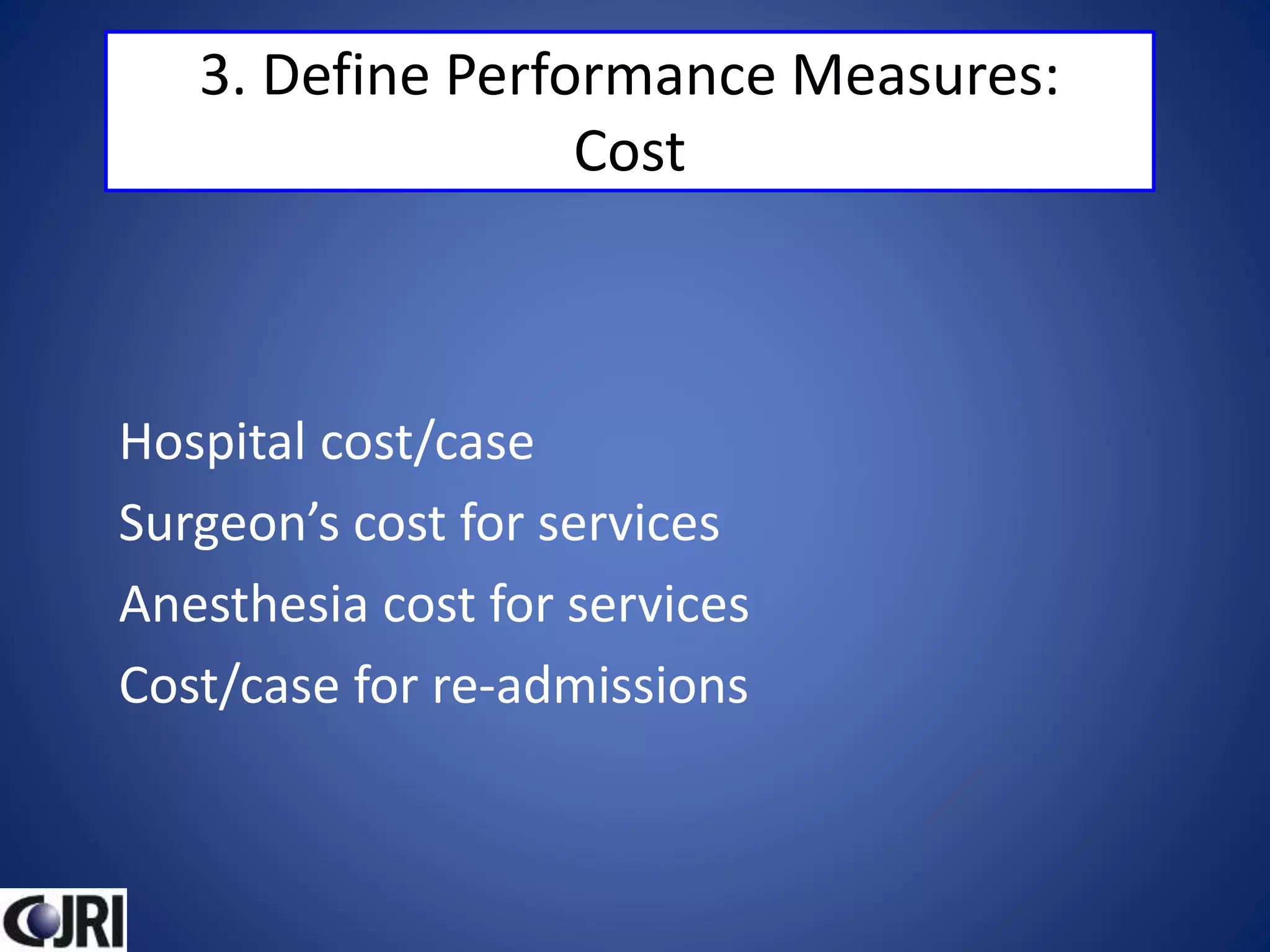
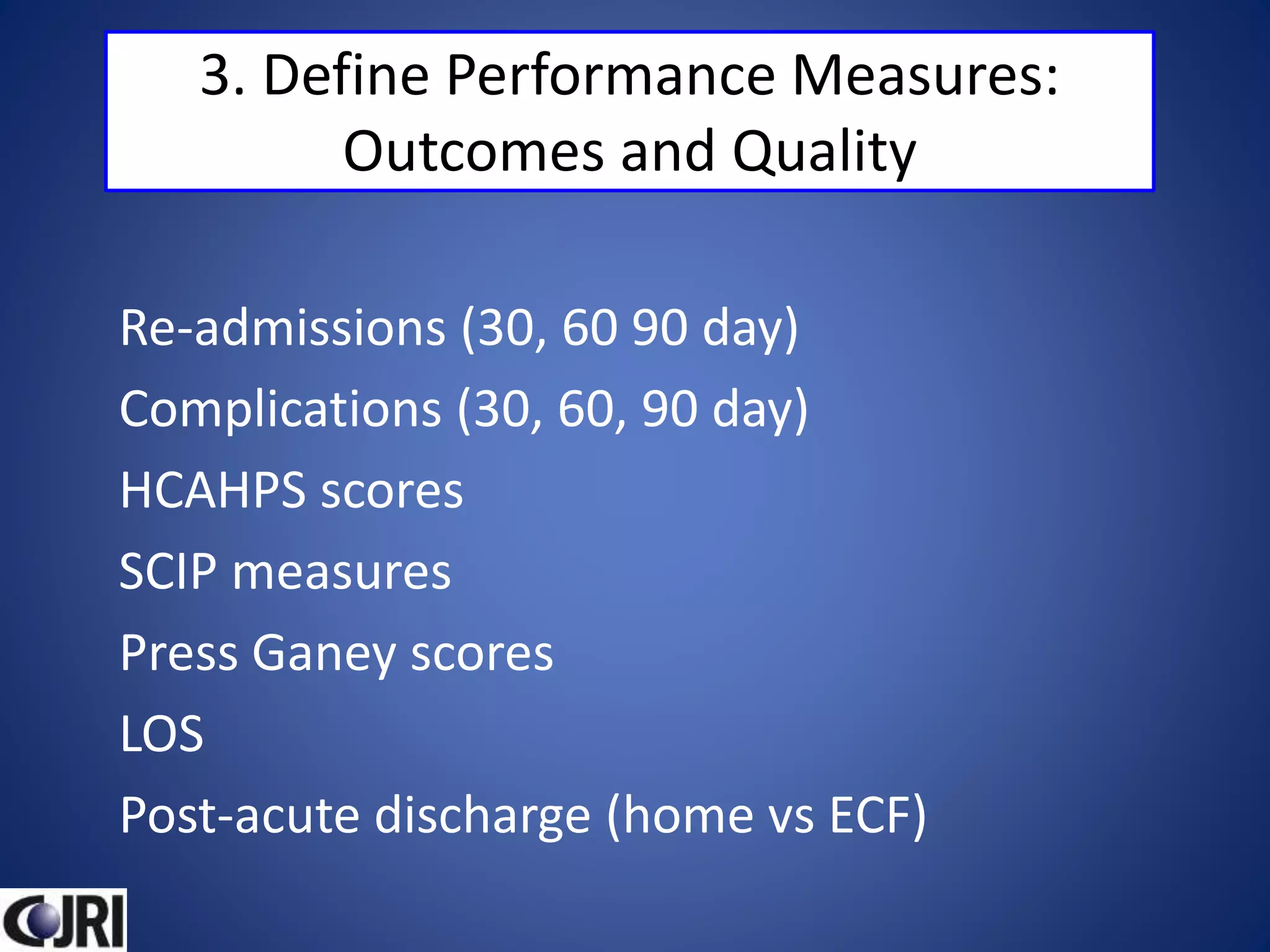
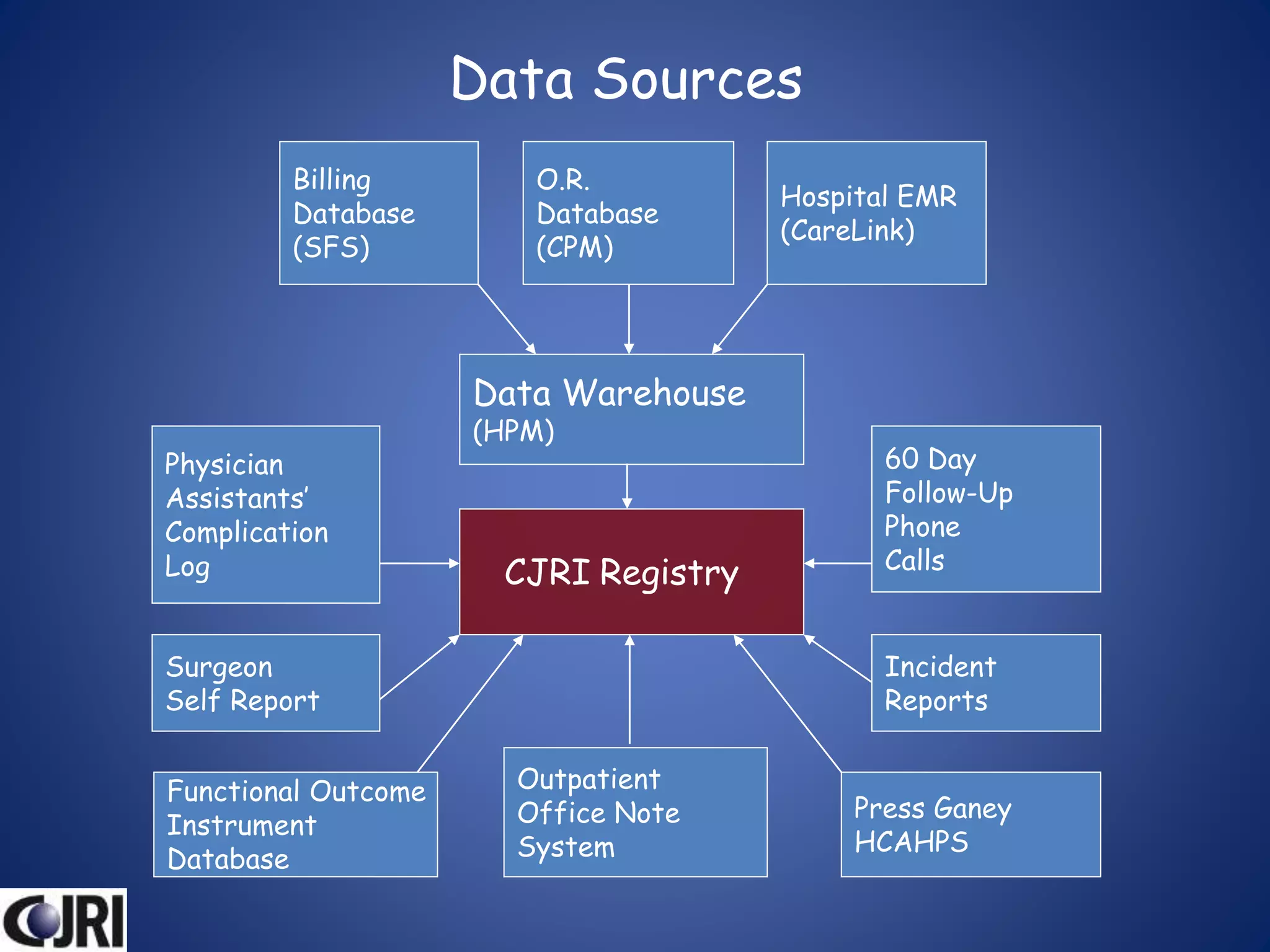
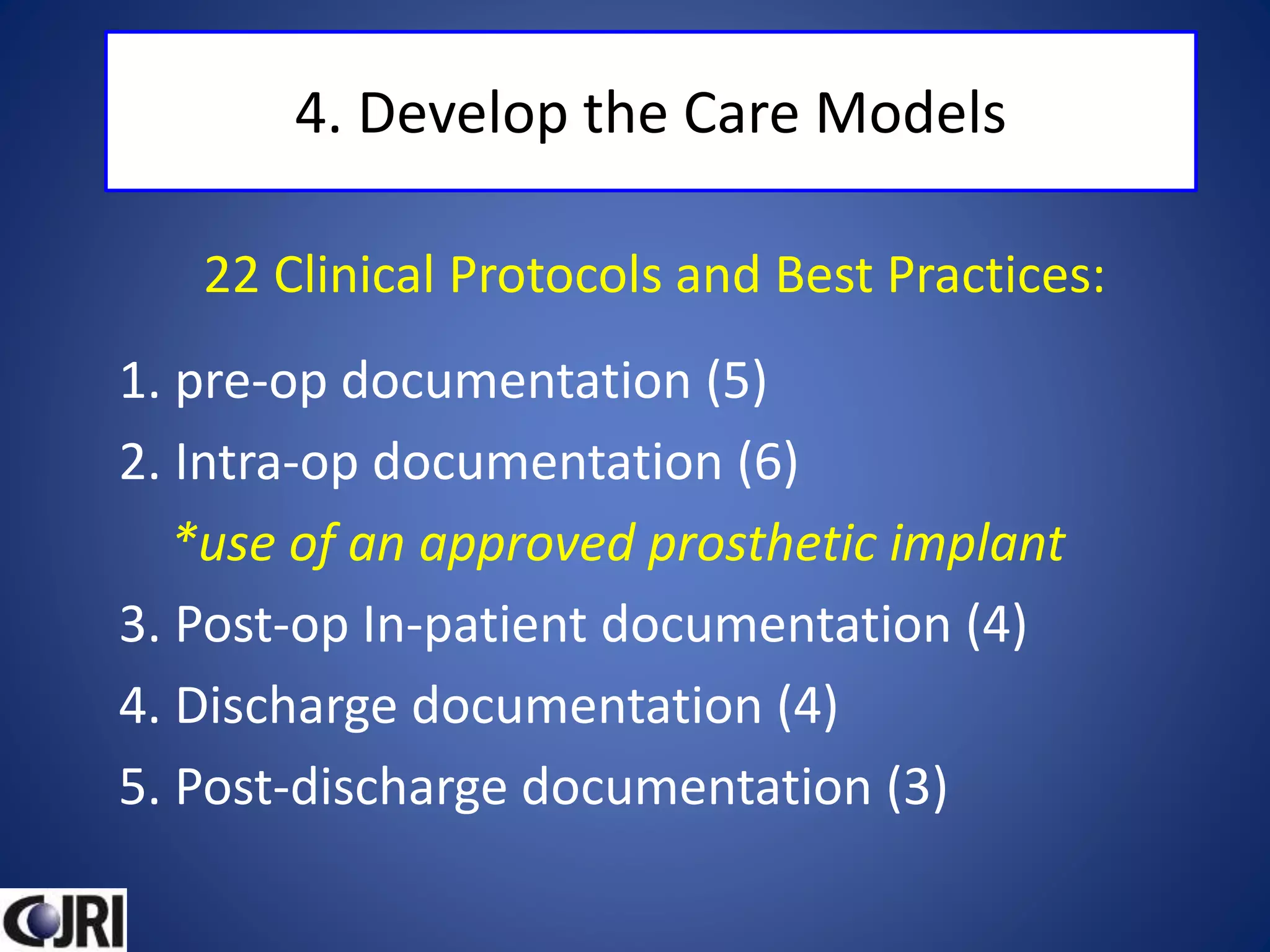
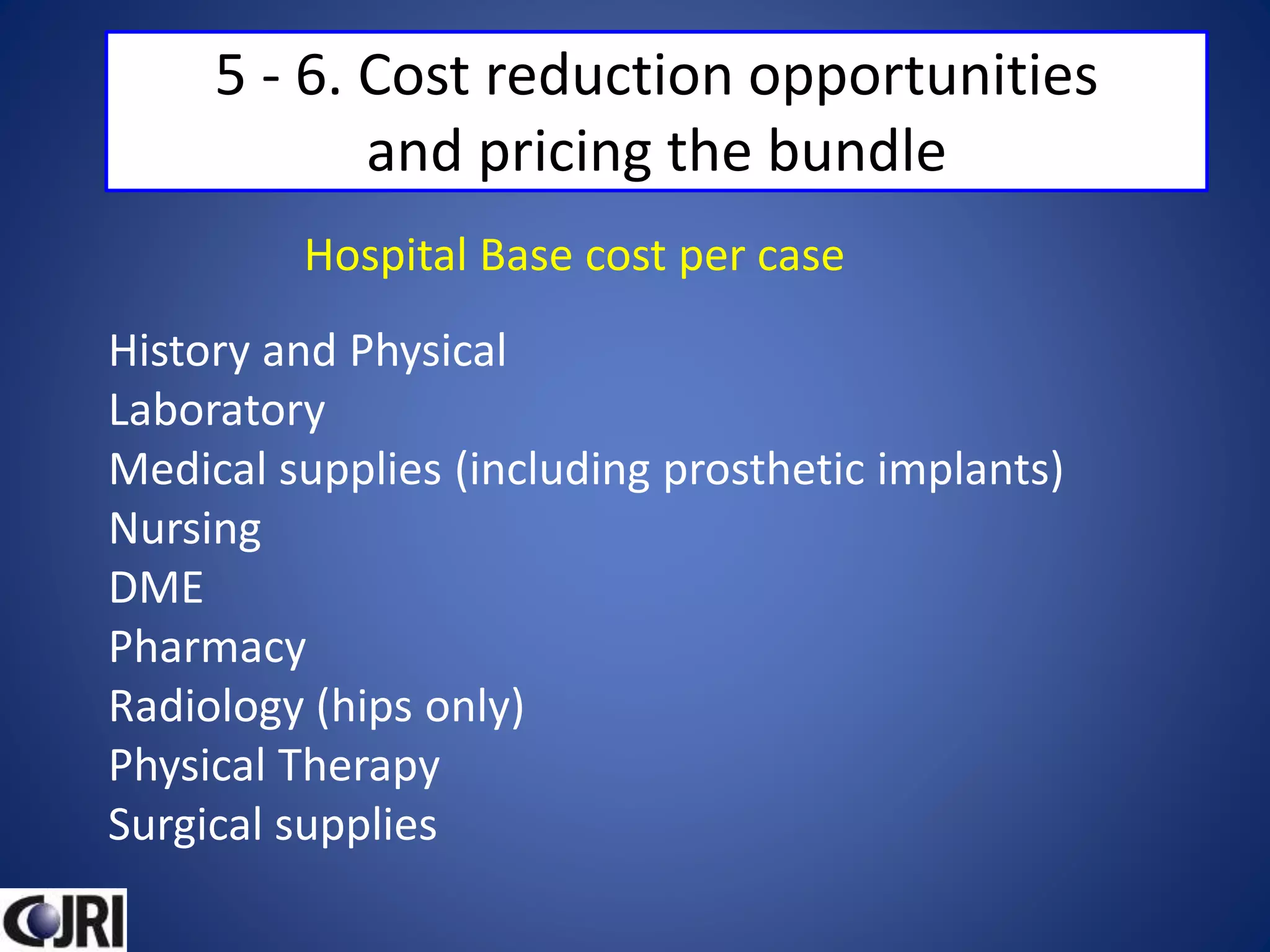
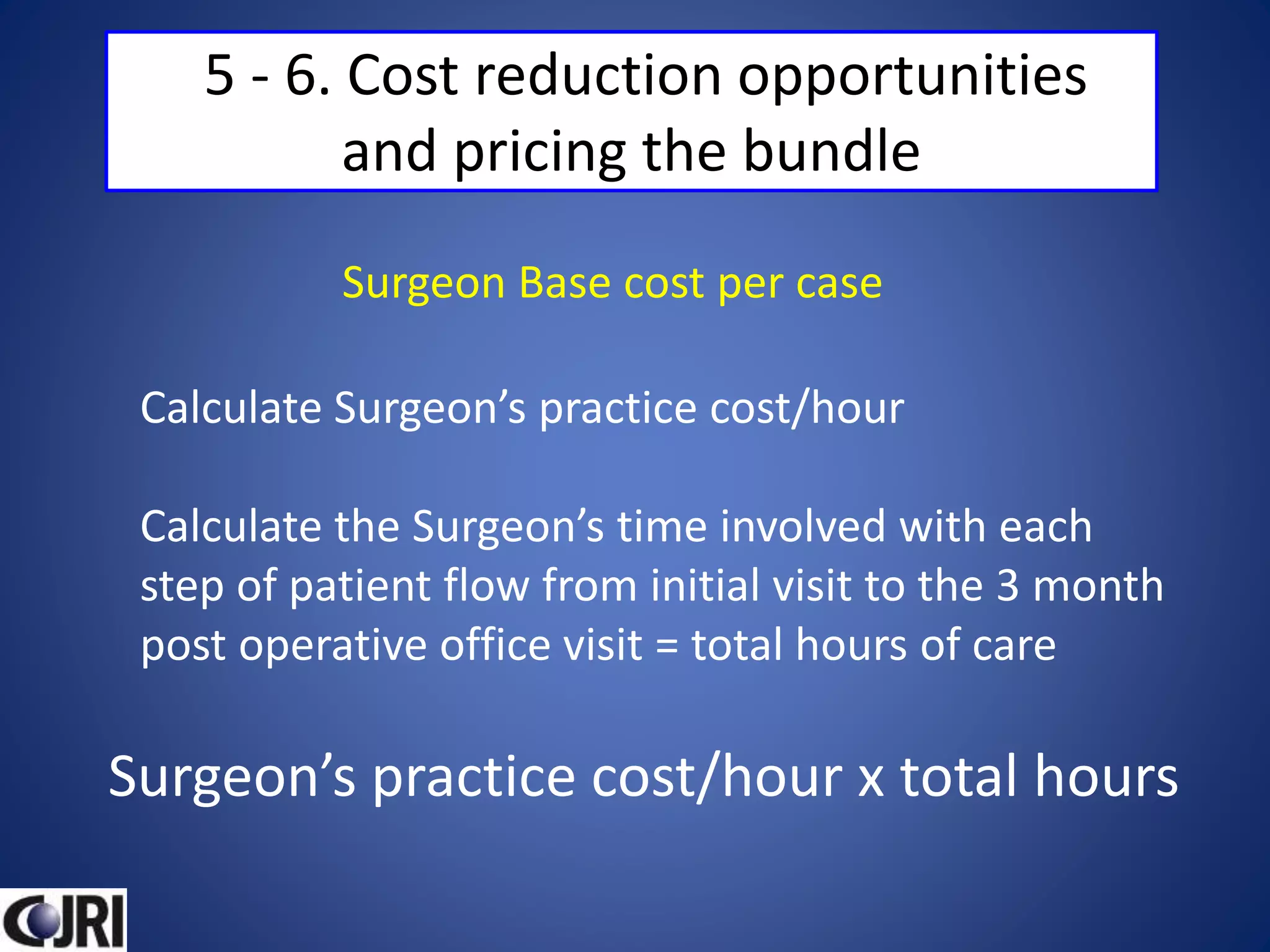
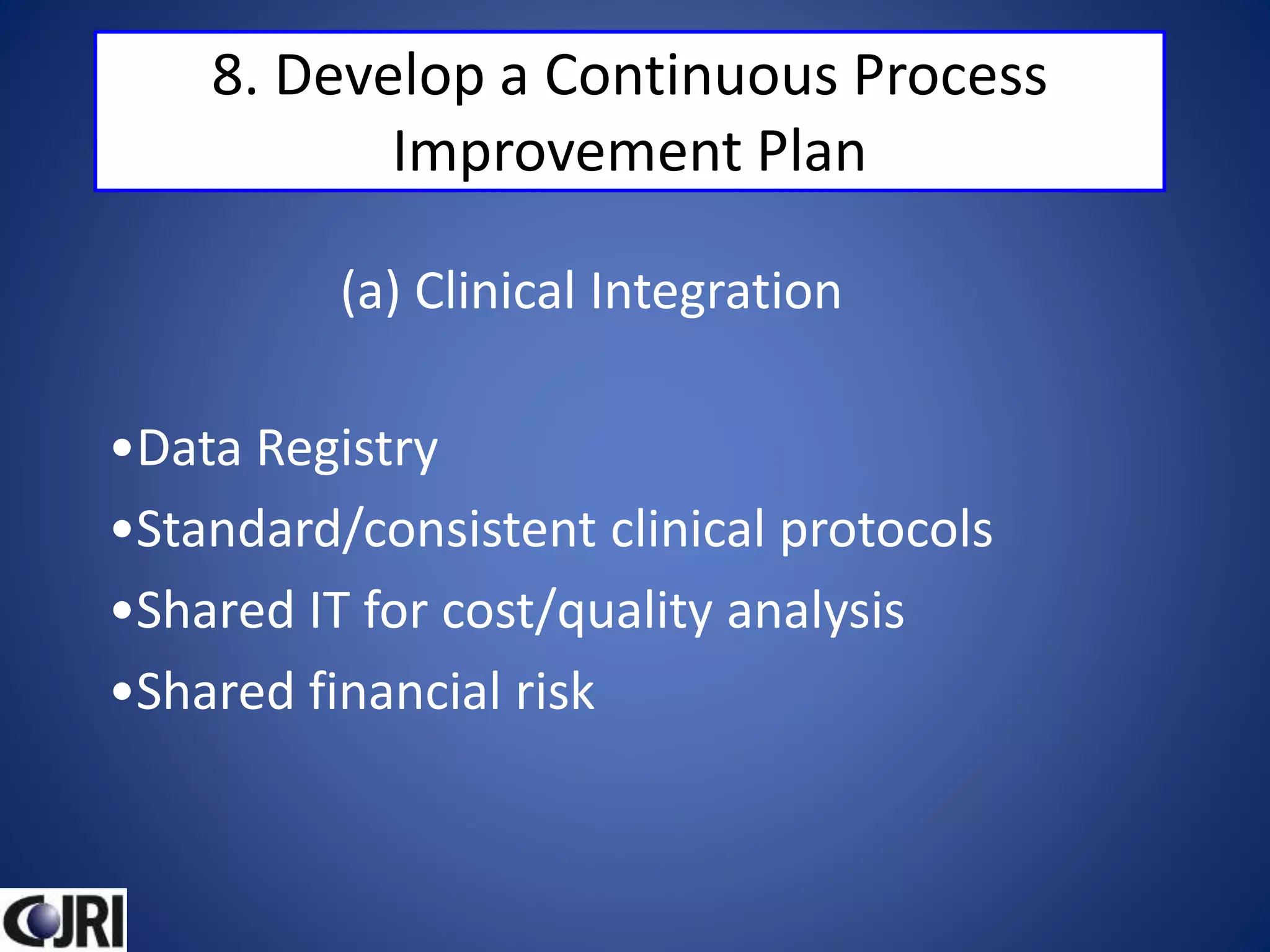
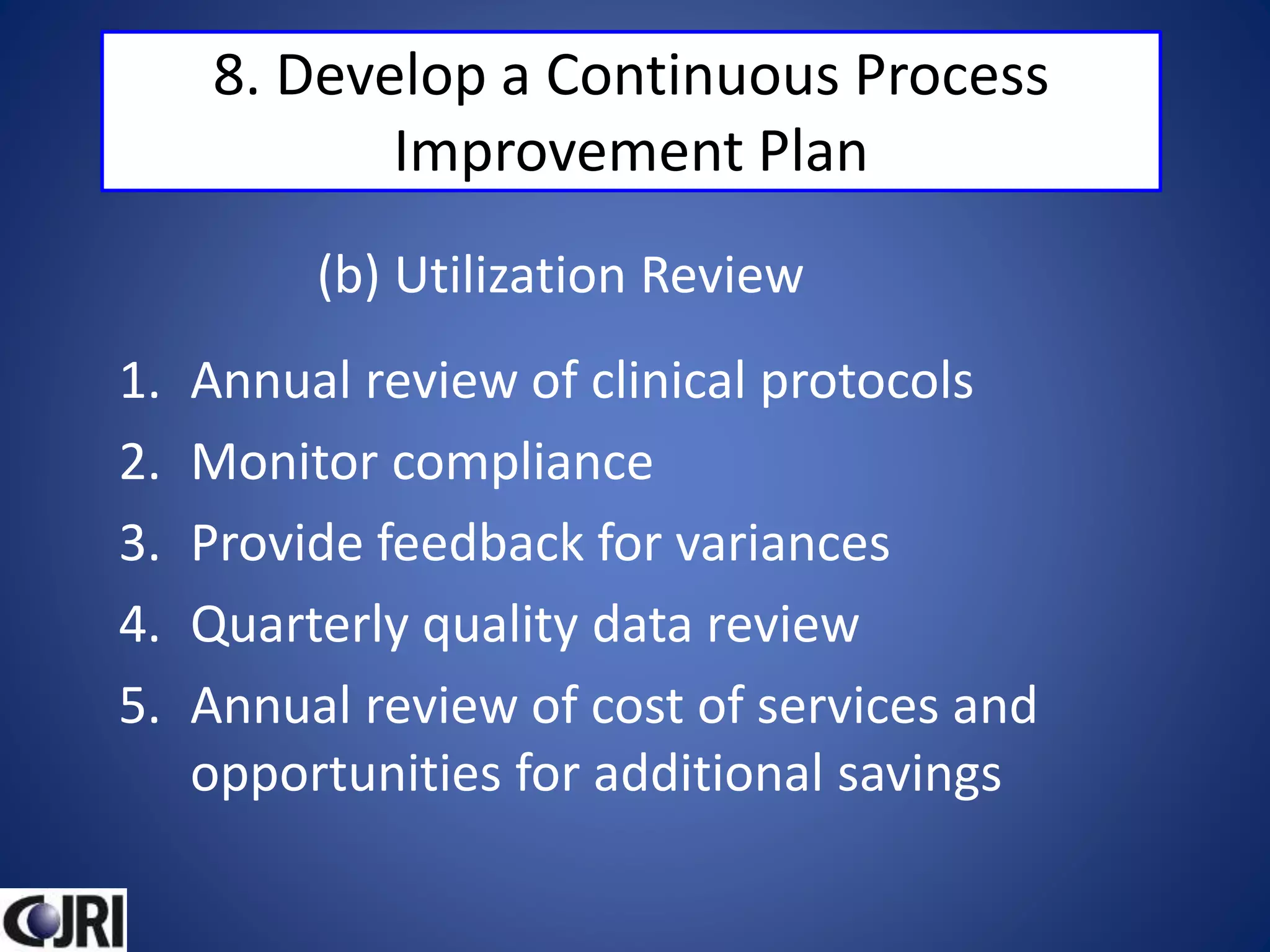
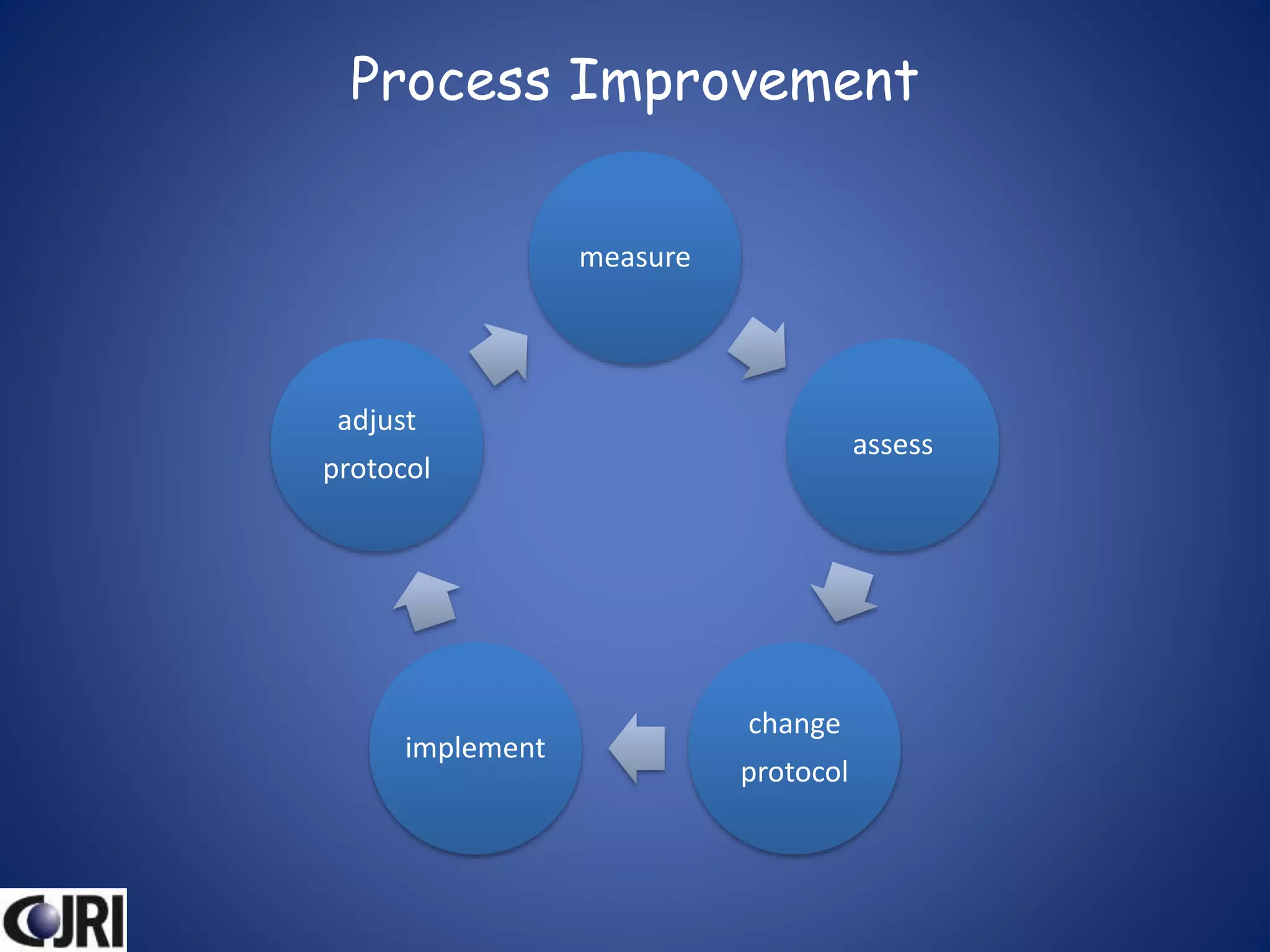
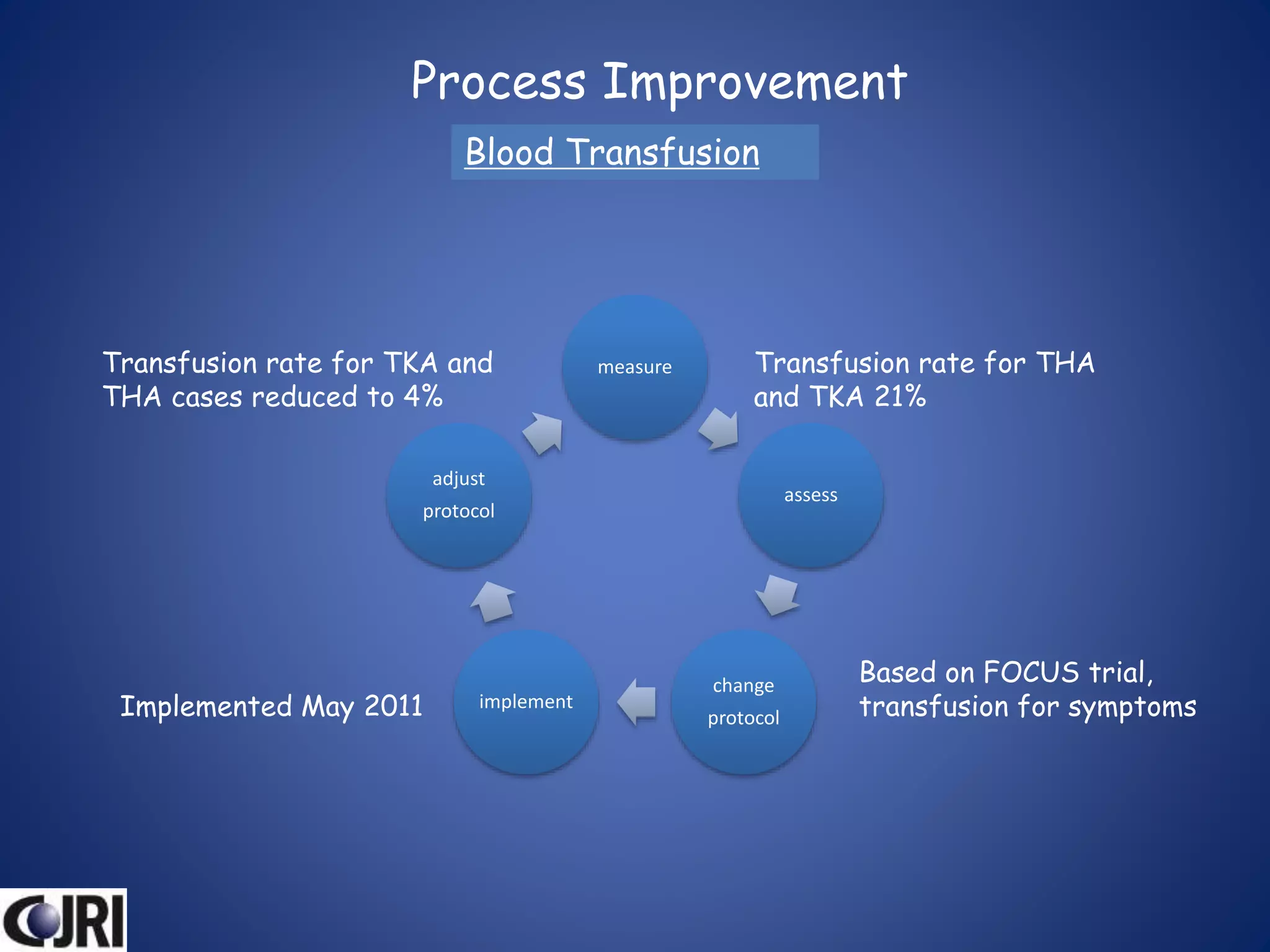
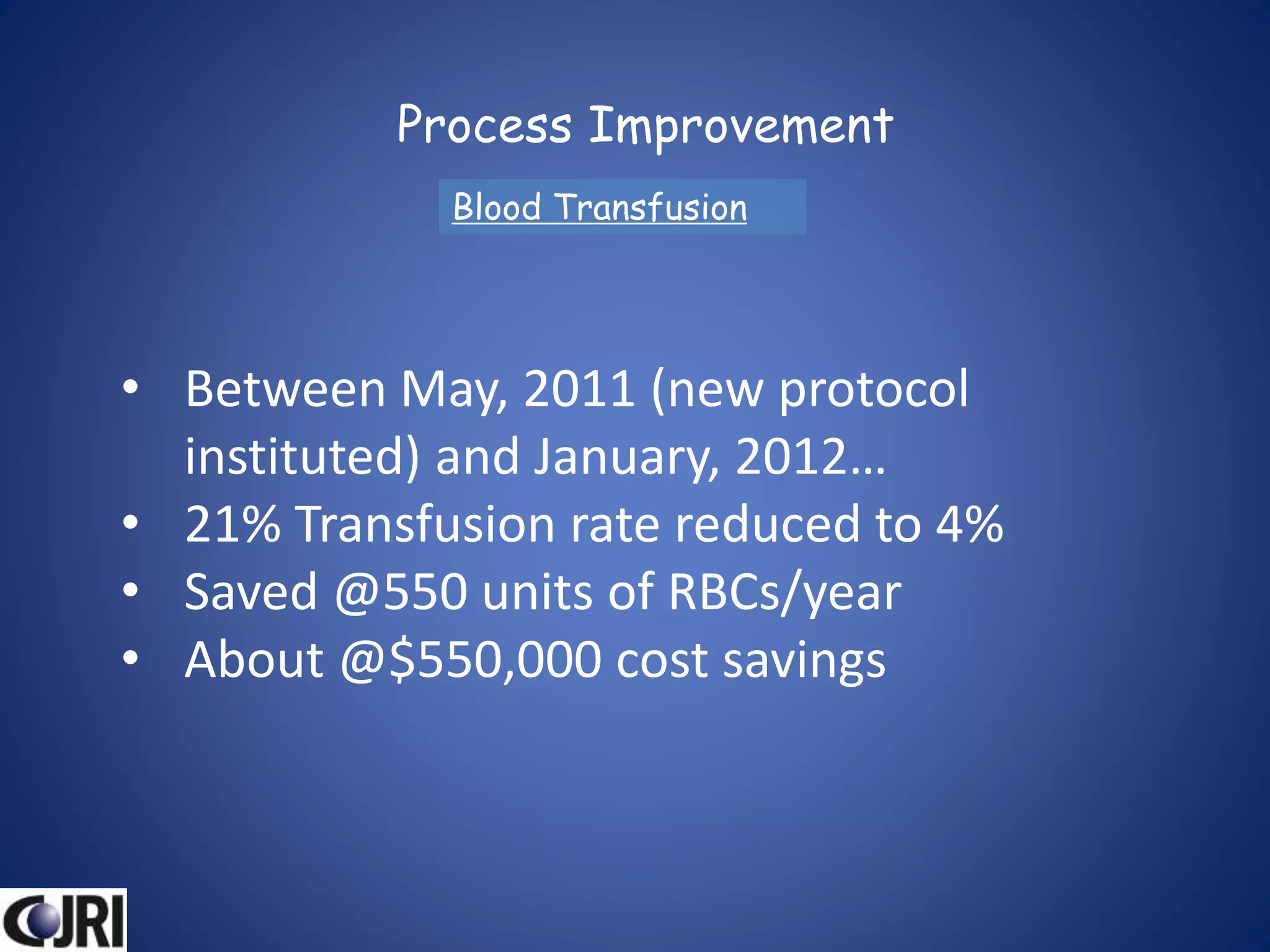
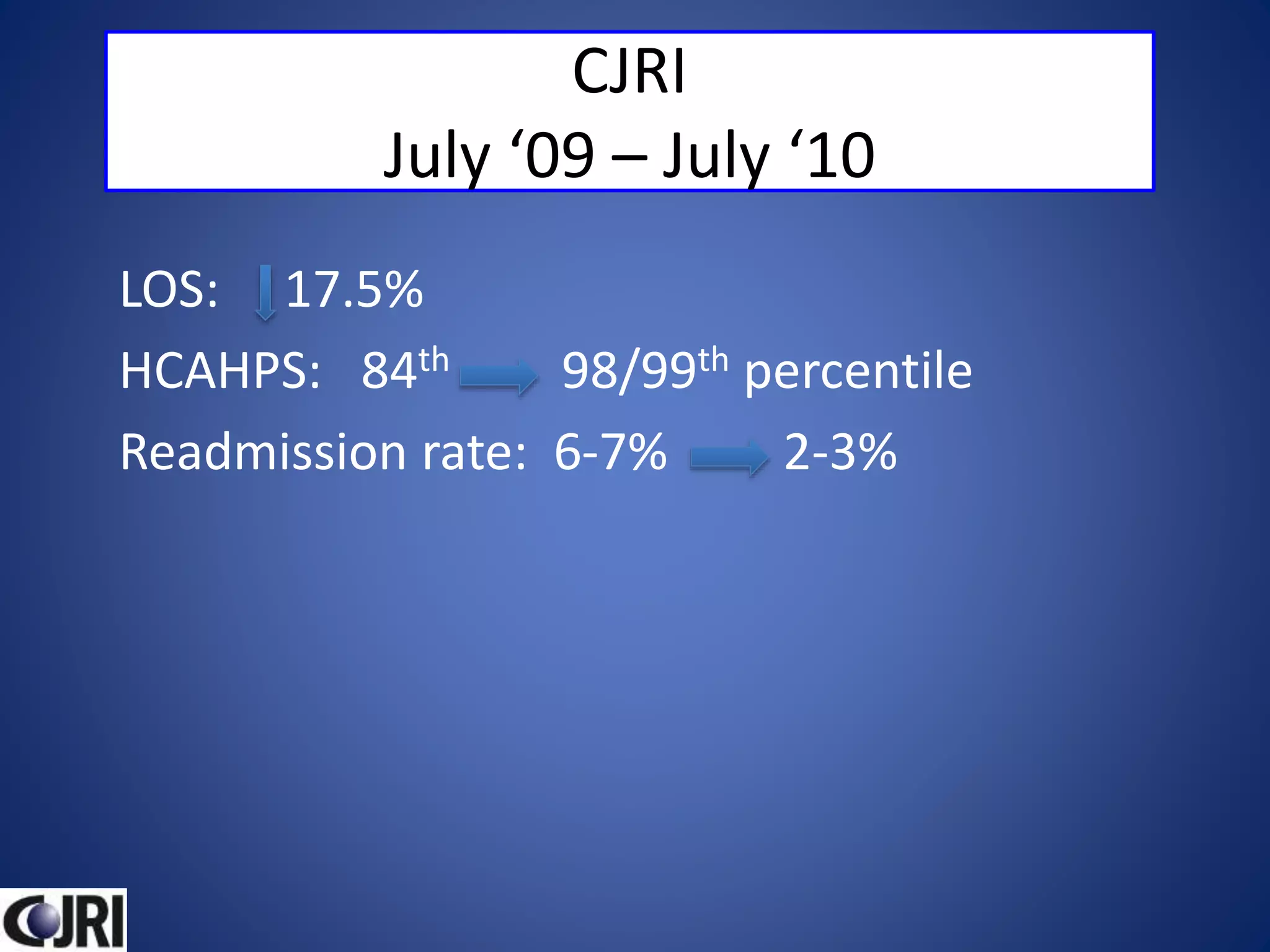
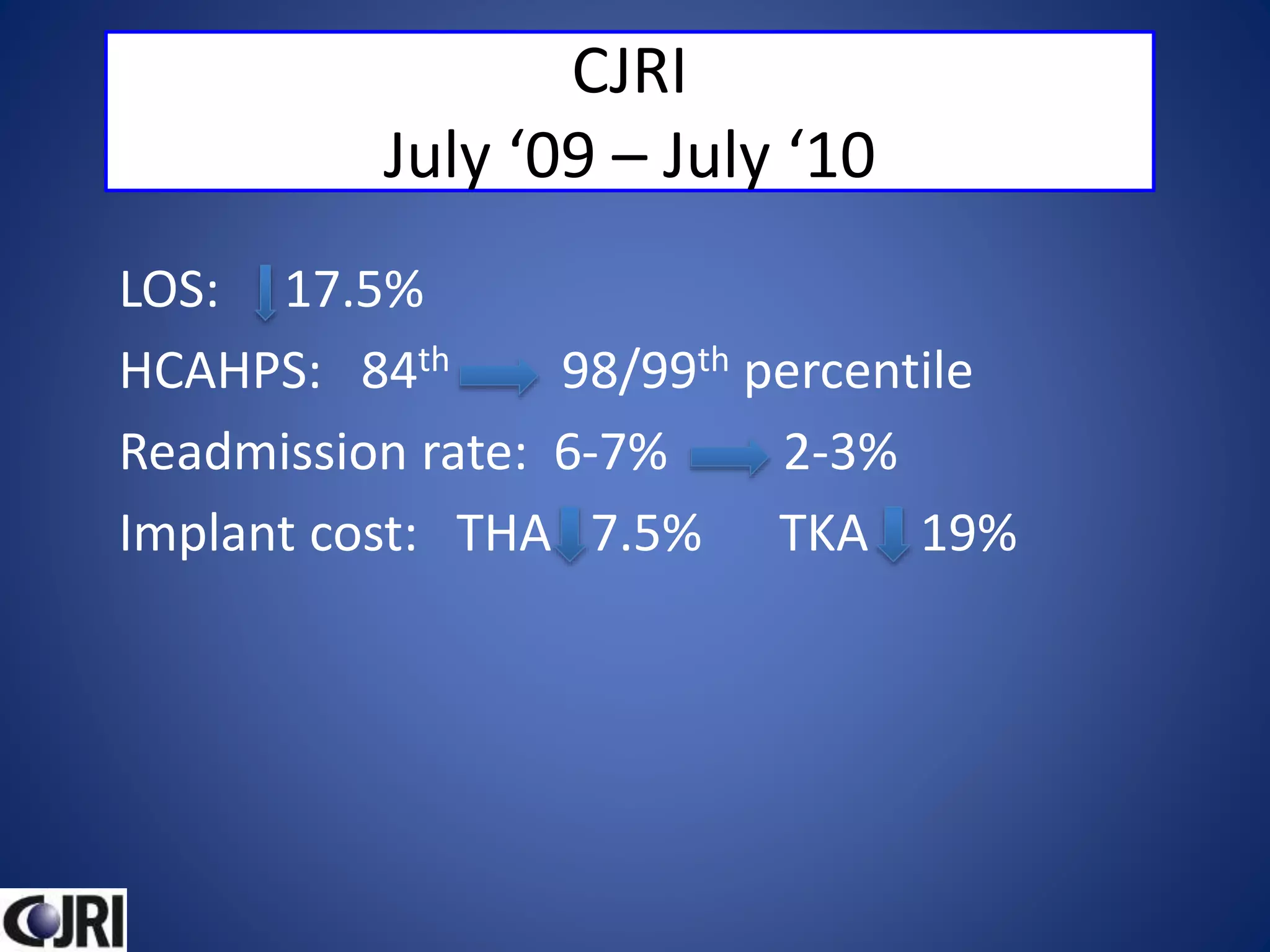
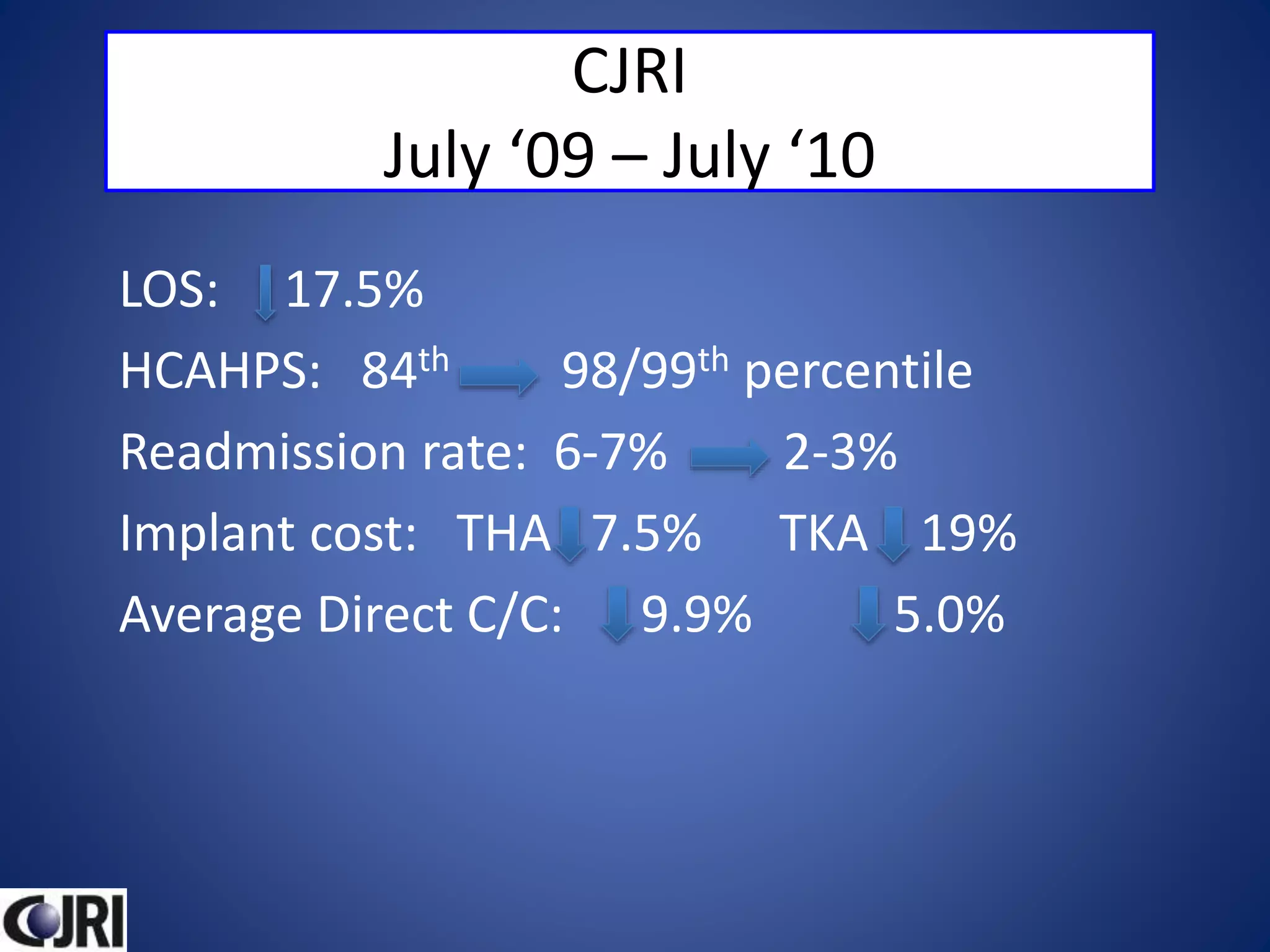
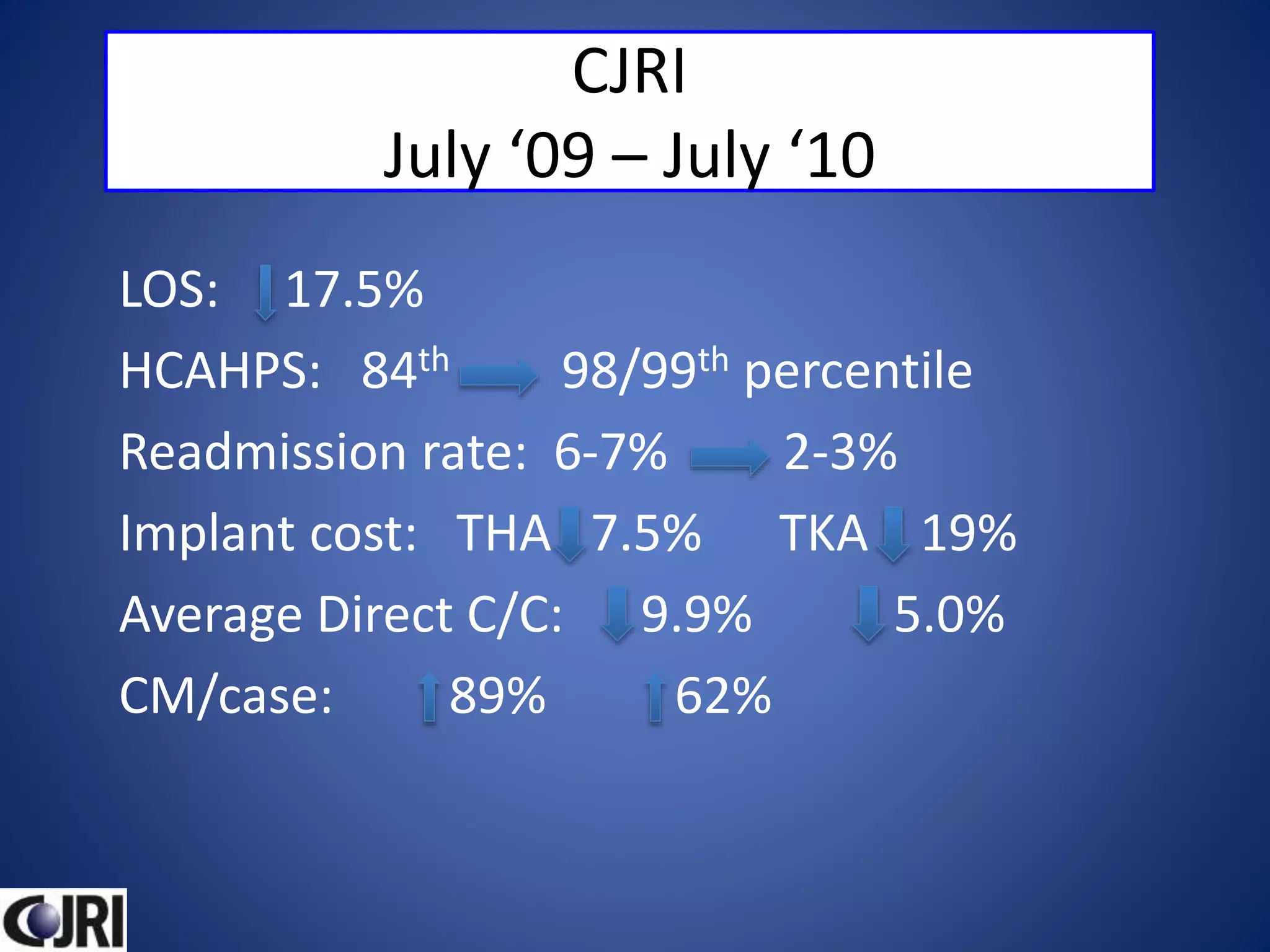
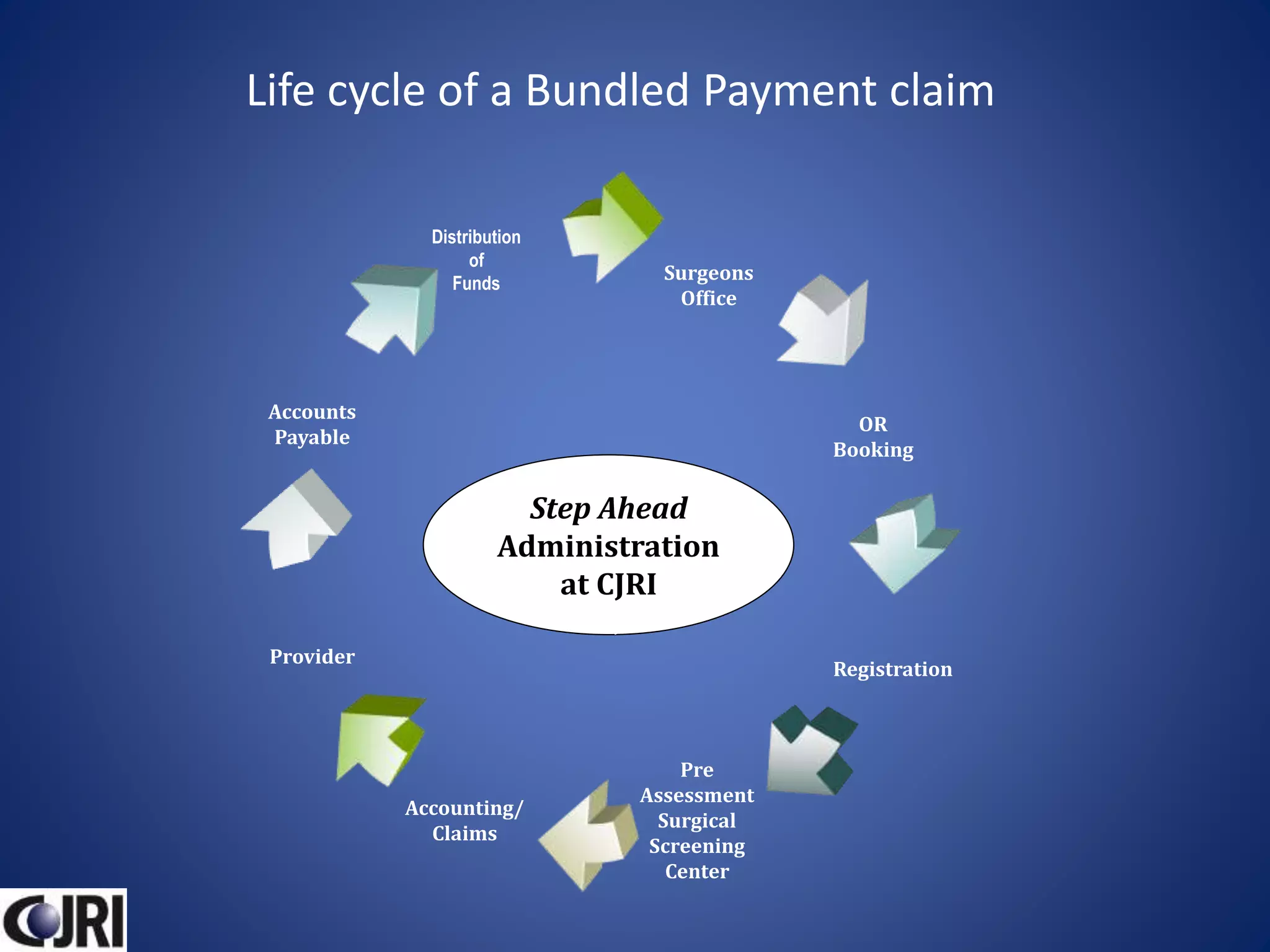
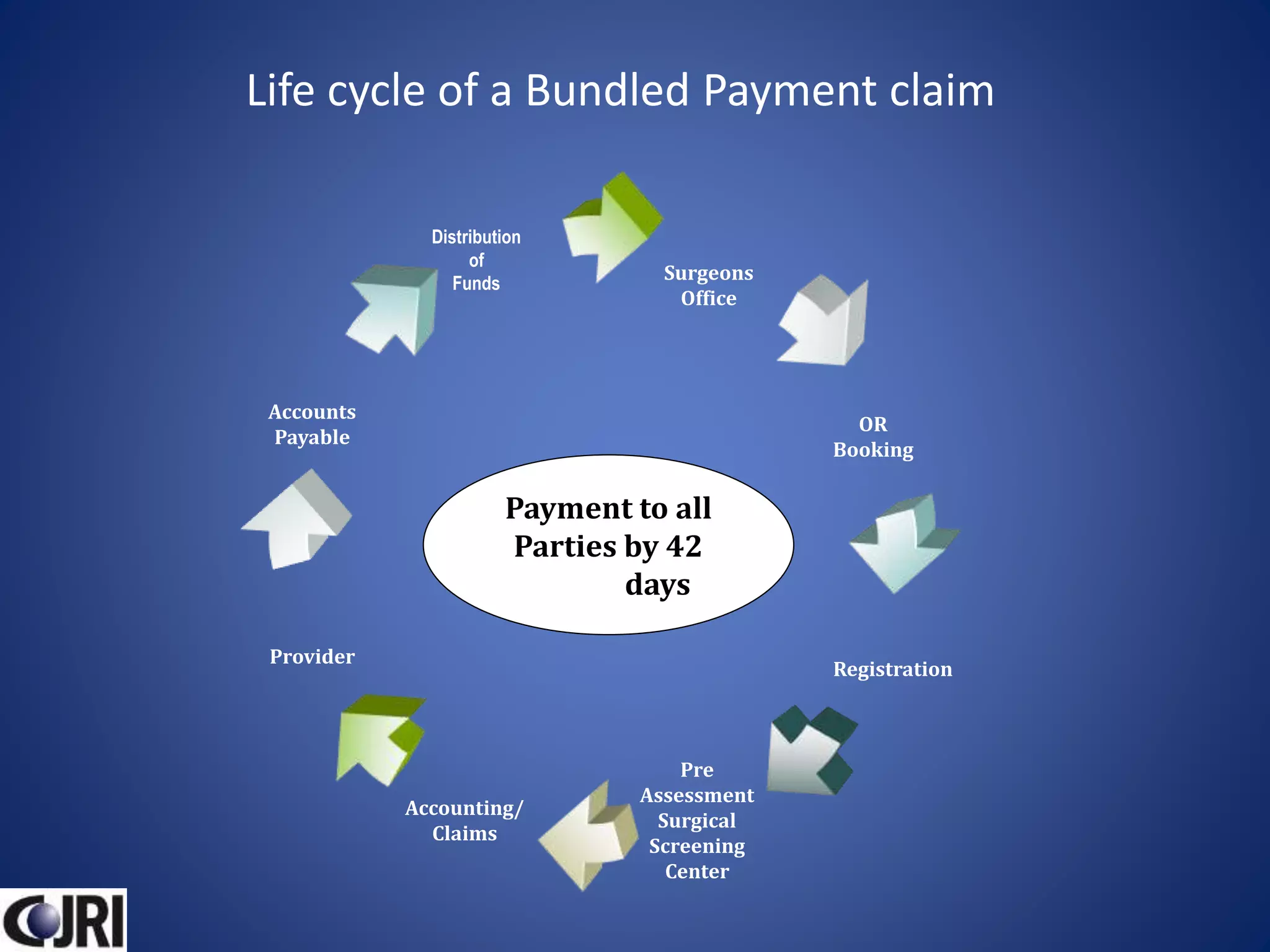
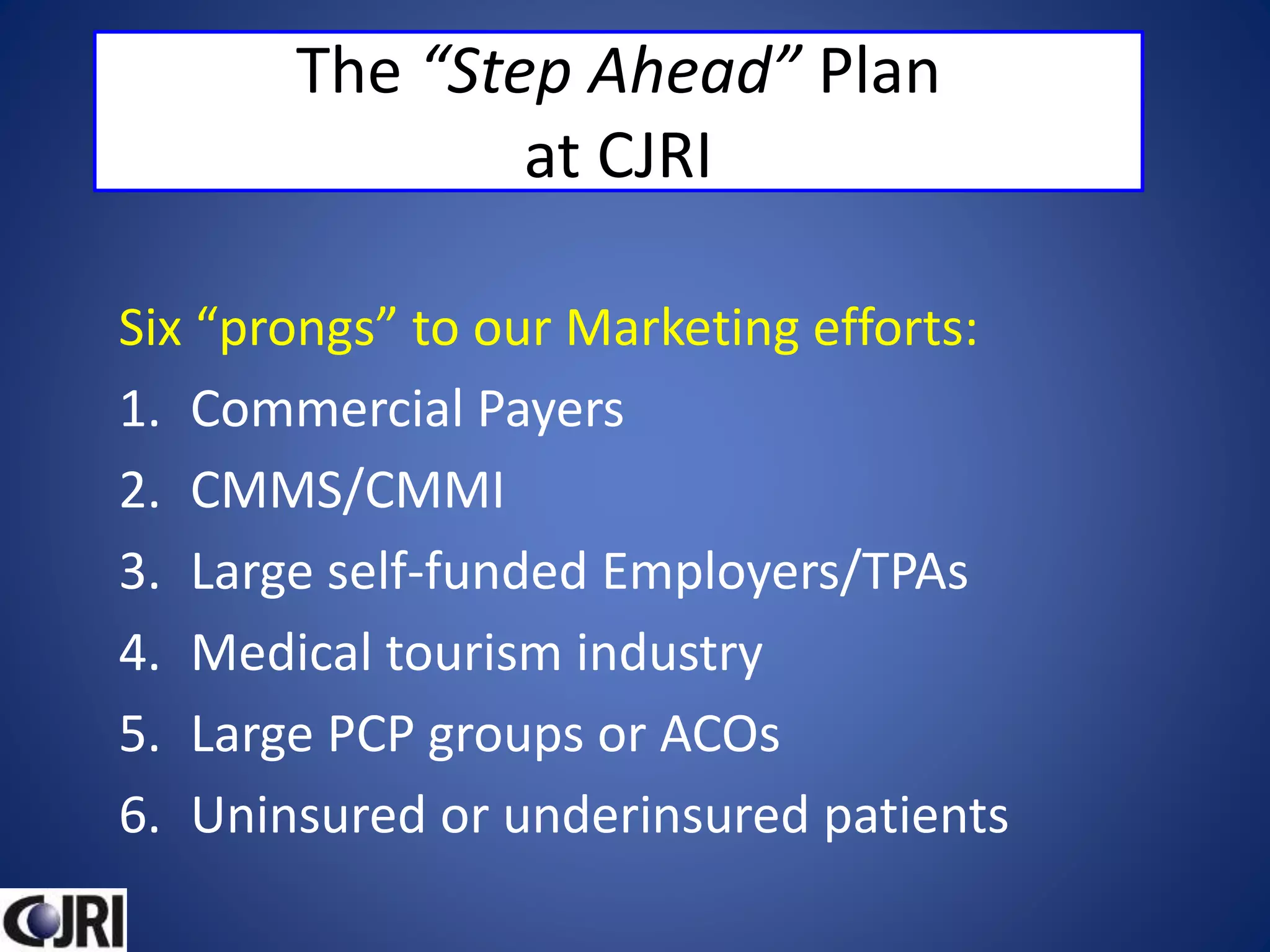
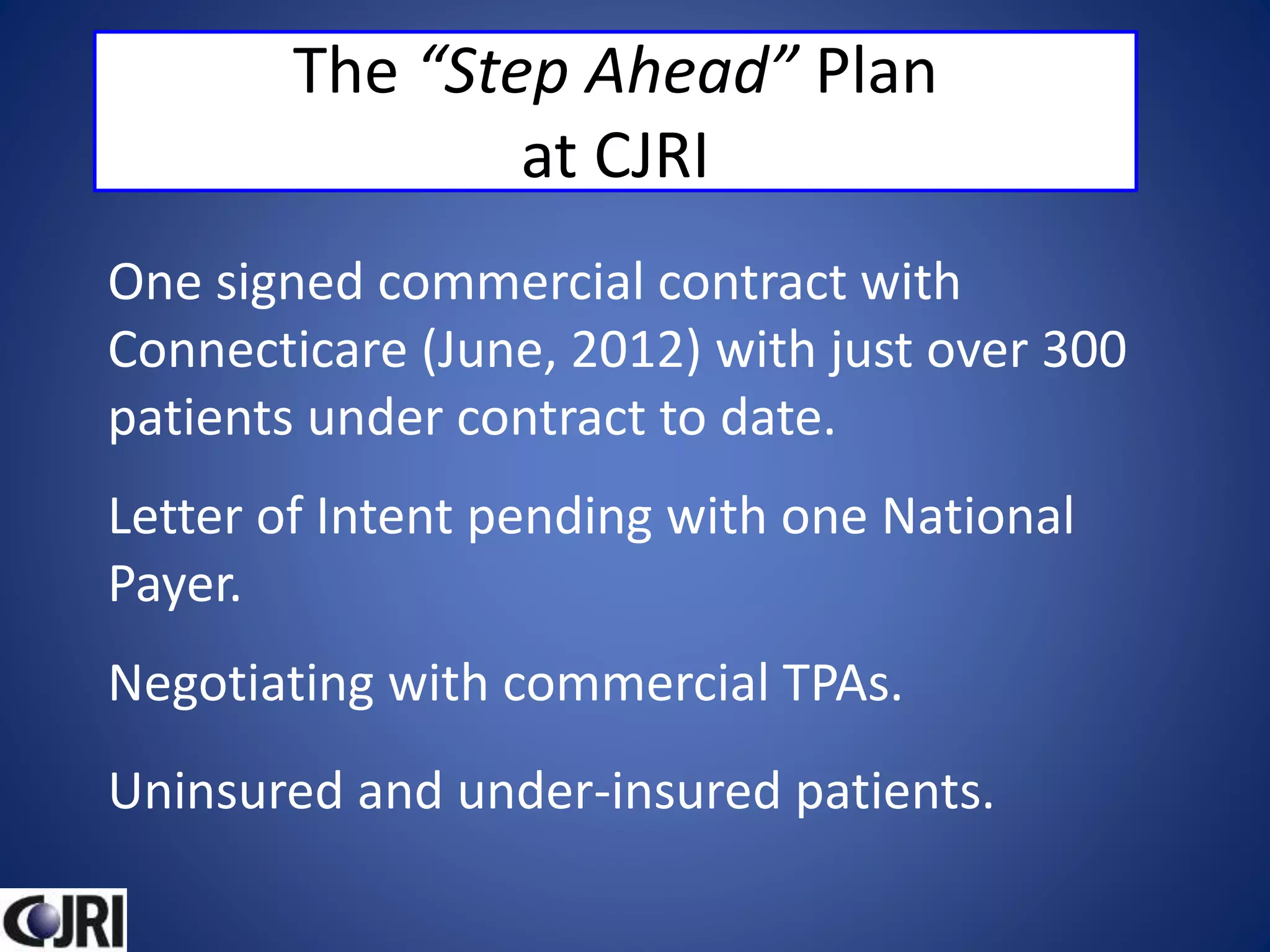
The document outlines the development and implementation of a bundled payment program at the Connecticut Joint Replacement Institute, highlighting key strategies for improving healthcare value through financial alignment between providers, payers, and patients. It emphasizes the importance of collaboration, data-driven decision-making, and integrated care models in order to enhance patient outcomes while controlling costs. Furthermore, it discusses potential pitfalls, risks, and advantages associated with transitioning to a bundled payment system in orthopedics.