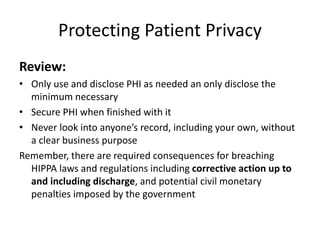
This document discusses patient privacy laws and regulations. It defines HIPAA and HITECH as laws governing the privacy and security of patient health information. It notes that HIPAA includes the Privacy Rule and Security Rule. The Omnibus Rule modified HIPAA to implement HITECH provisions. Organizations must implement policies to protect privacy and security, provide training, and designate privacy and security officials. The Breach Notification Rule requires reporting unauthorized access to patient information unless the risk is deemed low. The document concludes with a reminder to only access patient records as needed and to secure private health information.