This document provides information on the management of bone metastases. Some key points:
- Bone metastases are common in breast, prostate, and lung cancers and occur when cancer spreads from a primary site to the bone.
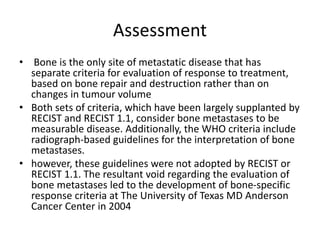
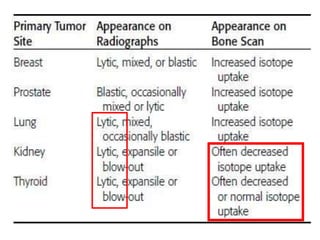
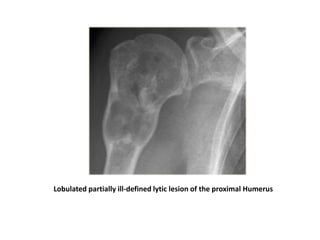
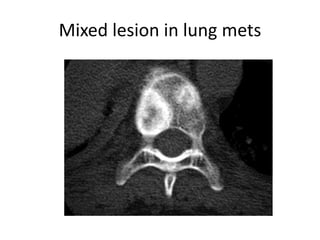
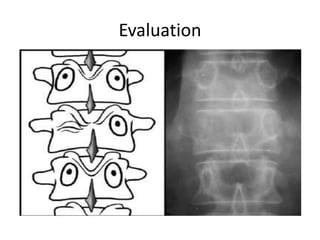
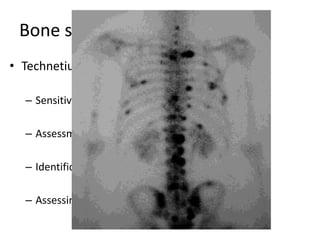
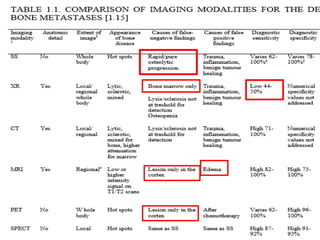
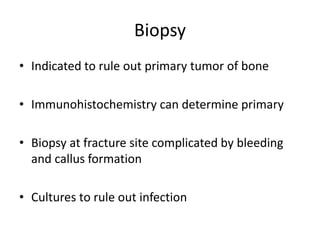
- Evaluation involves imaging like radiographs, CT, MRI, bone scans, and PET scans to determine the location and extent of bone lesions.
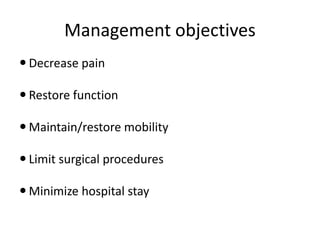
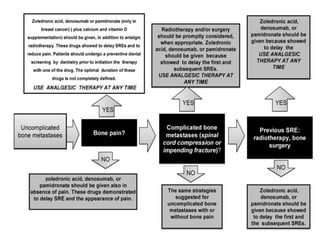
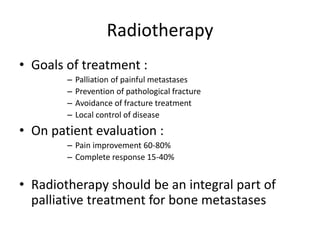
- Treatment objectives are to reduce pain, maintain mobility, and prevent fractures. Management includes bone-targeted agents like bisphosphonates, radiotherapy, surgery, and chemotherapy depending on the extent of disease.
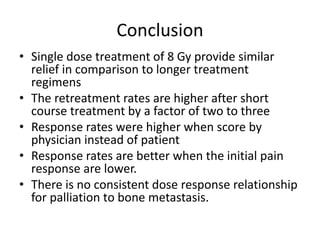
- Single fraction radiotherapy of 8 Gy provides similar pain relief as longer fractionated regimens but with higher retreatment rates. Multifraction
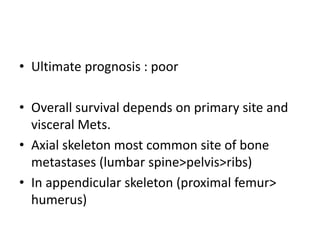

![Dutch Trial
• 1171 Patients with bone metastases from solid tumours primarily from
Breast[39%] , Prostate[29%] and Lung[23%] were randomize to two Arms 8
Gy/1# v/s 24 Gy/6 # .
• Painful areas has to be included in single treatment volume [spine(36%) and
pelvis(30%) was the most common sites].
• Malignant Melanoma and Renal cell carcinoma Excluded.
• Primary End Point : Patient assessment for pain relief on 11 point scale
• Median pain score was 6.3 with lowest being 2.
• Half of the patients was receiving Narcotics or systemic therapy
• Results
• Median survival 30 wks.
• Overall response [71%] , complete response[35%].
• Response time 4-6 wks.
• Rate of pathologic fracture 4% v/s 2%.
• Median time to fracture similar in both arms
• Retreatment 25% v/s 7 %.
– Retreatment was given at lower score in single fraction arm indicating the
reluctance to give retreatment after higher doses.
• Higher complete response rates and lower retreatment rates were observed
in Breast and Prostate in comparison to Lung.](https://image.slidesharecdn.com/bonemetsfinal-170824120652/85/management-of-bone-secondries-30-320.jpg)
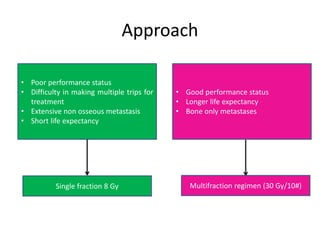
![RTOG 9714 Trial
Randomized Trial of Palliative Radiation Therapy For Osseous Metastases: A Study of Palliation of Symptoms
and Quality of Life For Osseous Metastases: A Study of Palliation of Symptoms and Quality of Life
• 938 Patients with painful metastases from breast and prostate,
Randomize to 8 Gy/1# v/s 30 Gy/10#.
• Inclusion criteria
– Minimum pain score 5 or higher
– Narcotic dose > 60 mg of Morphine.
– If multiple painful sites present they should be covered within 3 treatment fields
• Results (3 months post treatment)
– Median survival was 9.3 months
– Complete response[17%], partial response[49%].
– Rates of stable or progressive pain score identical.
– Rates of Narcotic use identical
– Retreatment 18% v/s 9 %.
– No difference in rate of pathological fracture [5% v/s 4%]
– Acute toxicity (grade 2-4) , 10% vs 17% (p value 0.002).
• Konski et Al. showed that married man and single or married woman were
more likely to et retreatment in 8 Gy arm v/s 30 Gy arm in comparison to single
males in which the rates of retreatment was higher in both arms indicating the
role of social support in patient outcome.](https://image.slidesharecdn.com/bonemetsfinal-170824120652/85/management-of-bone-secondries-31-320.jpg)
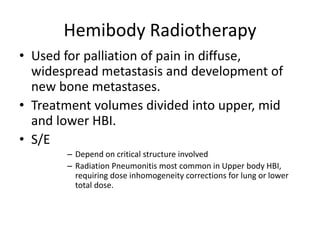
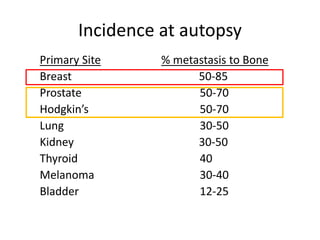
![• Doses :
– Single Fraction Regimens :
• Mid and Lower HBI , MTD : 8 Gy
• Upper HBI , MTD : 6 Gy with corrections and 7 Gy without
corrections.[1]
– Multi fraction Regimen :
• Rationale is to reduce the acute toxicities
• RTOG 88-08: 2.5 Gy to 4 Gy to total dose of 8 to 20 Gy with MTD of
17.5 Gy in 7#
• IAEA study : 3 Gy BD for 2 days or 3 Gy daily for 5 days and 4 Gy
daily for 2 days.
• s/e : Gastrointestinal and hematologic
• Multifraction regimen is of no additional benefit in
comparison of Single dose regimen if delivered with
adequate premedication.[2]
[1] RTOG 78-10 trial
[2] sarin R , budrukar A : Efficacy toxicity and cost effectiveness of single versus fractionated Hemi body
RT : Int J of Rad Onc Biol Phy 2002;52;1146.](https://image.slidesharecdn.com/bonemetsfinal-170824120652/85/management-of-bone-secondries-35-320.jpg)