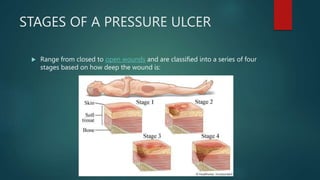
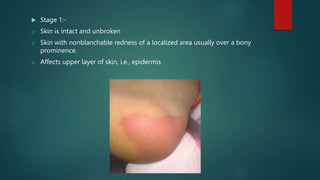
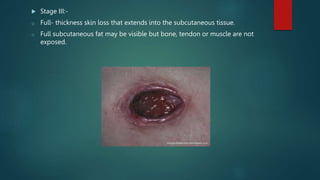
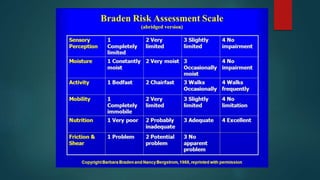
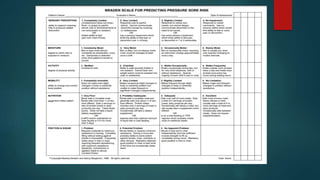
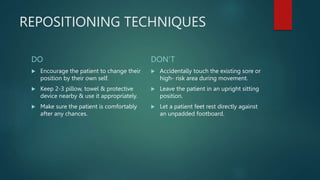
Pressure ulcers, or bed sores, are localized damage to skin and underlying tissues caused by prolonged pressure, commonly found over bony prominences. The document outlines the causes, stages, and prevention techniques for pressure ulcers, emphasizing the importance of skin assessment and proper care strategies to mitigate risks. Key interventions include repositioning, maintaining skin hygiene, and ensuring nutritional balance.