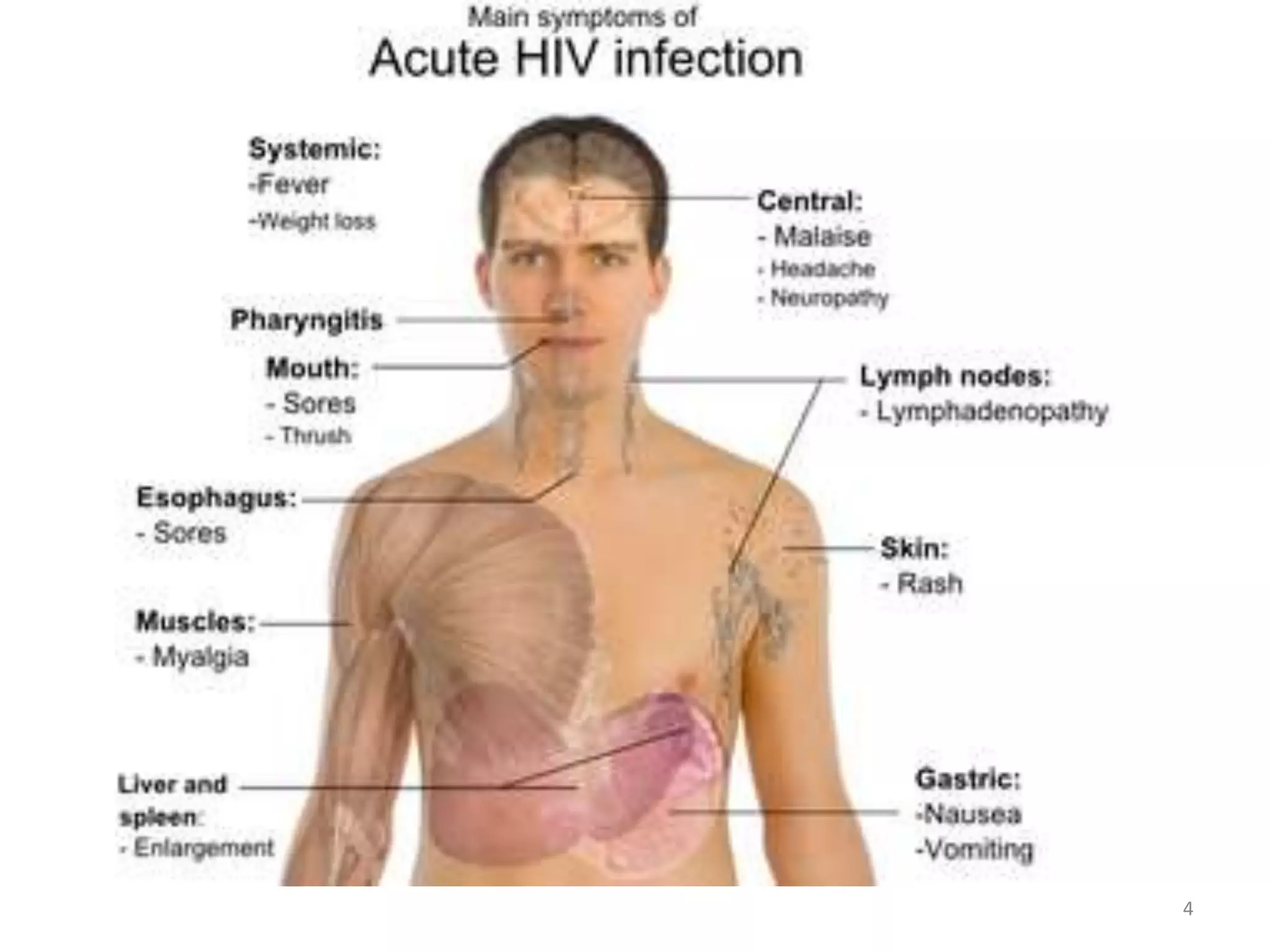
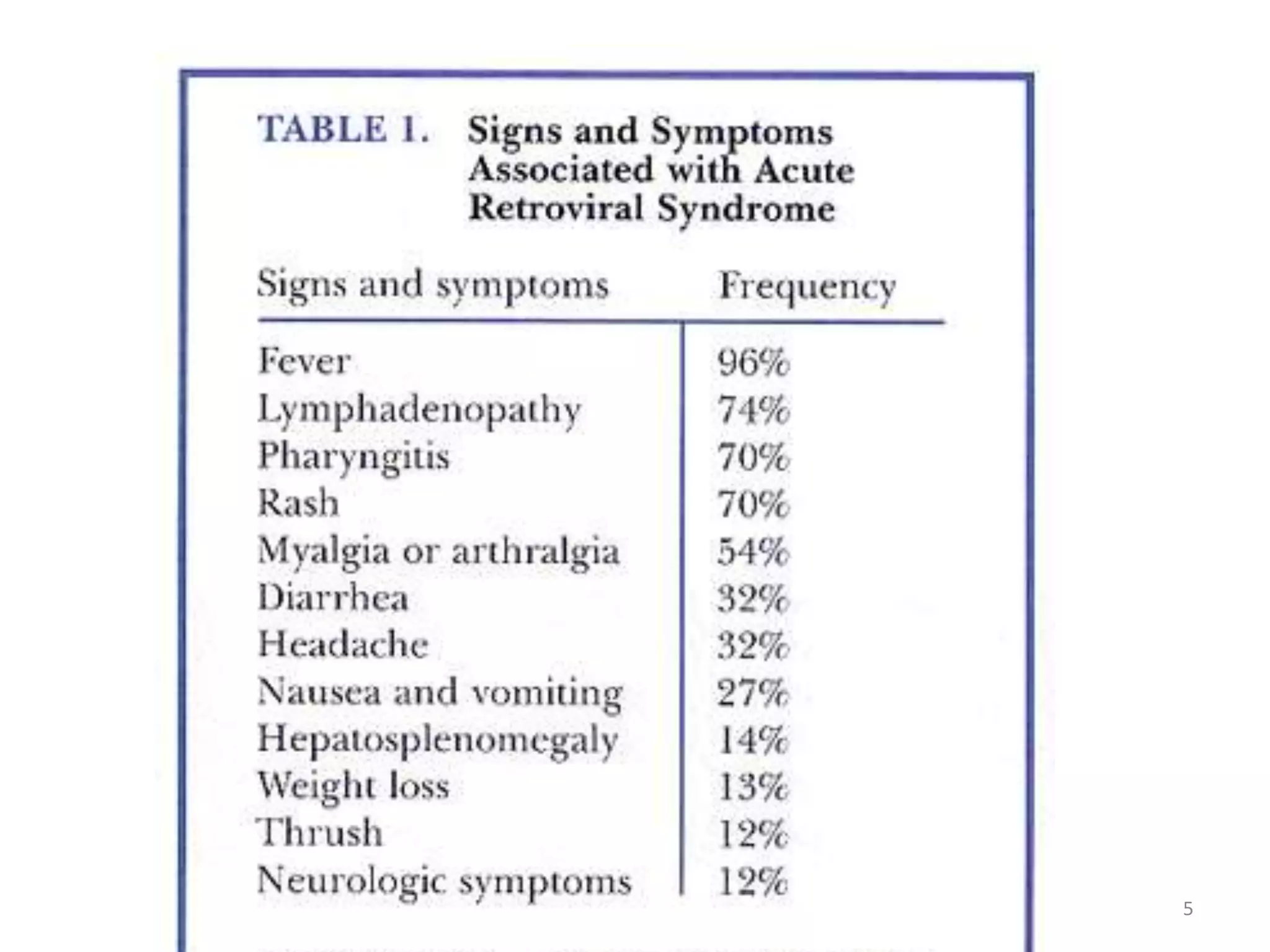
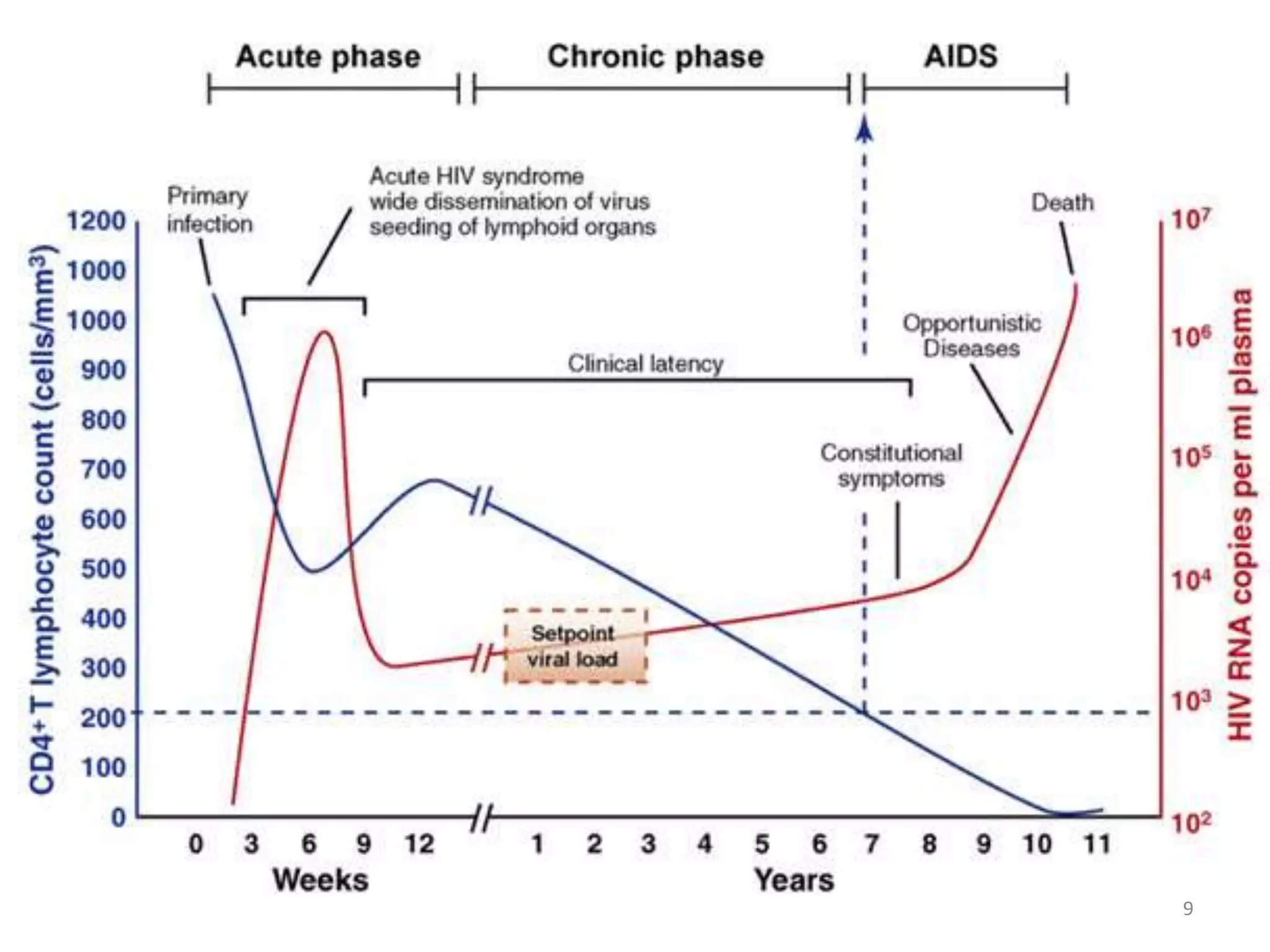
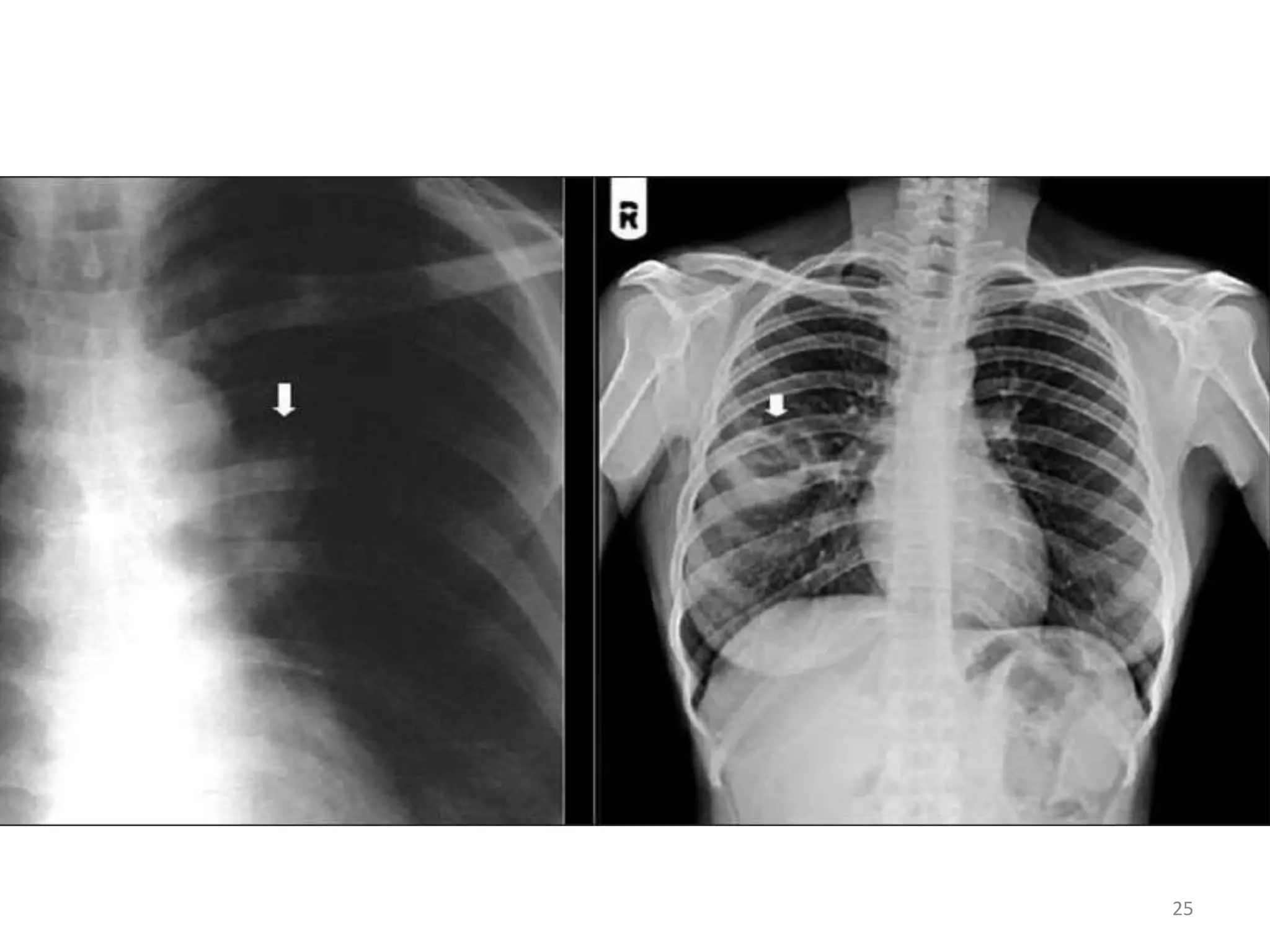
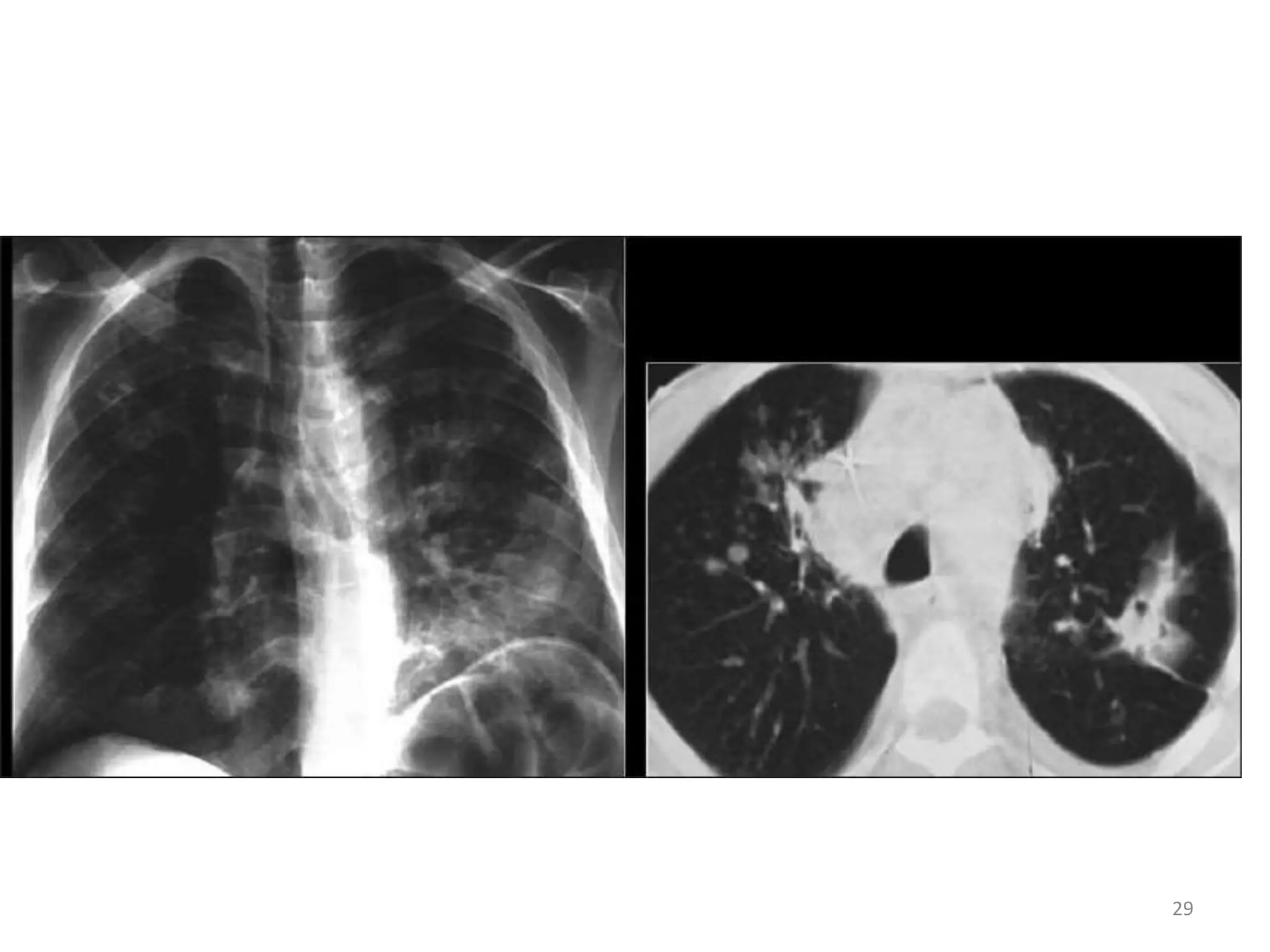
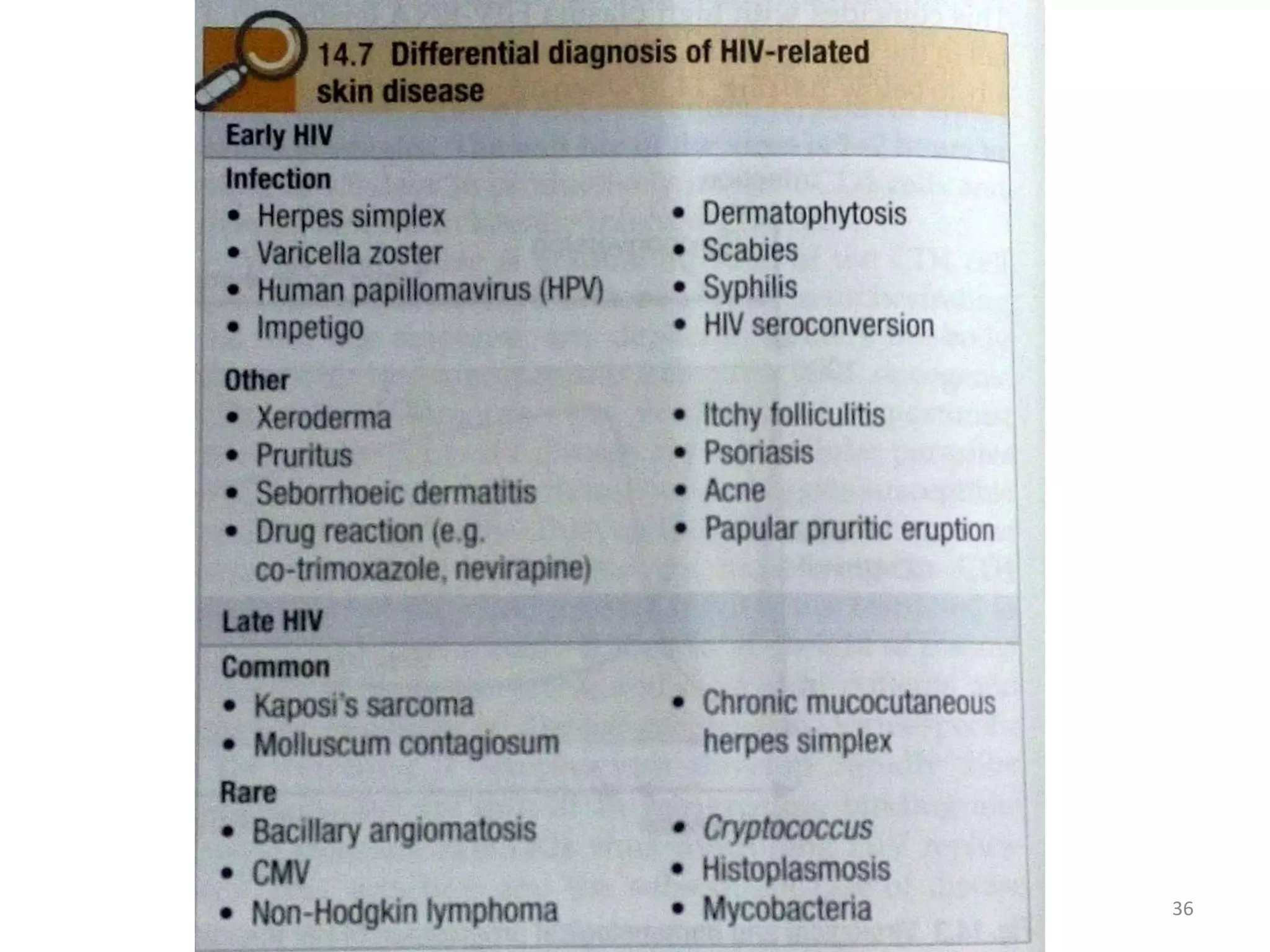
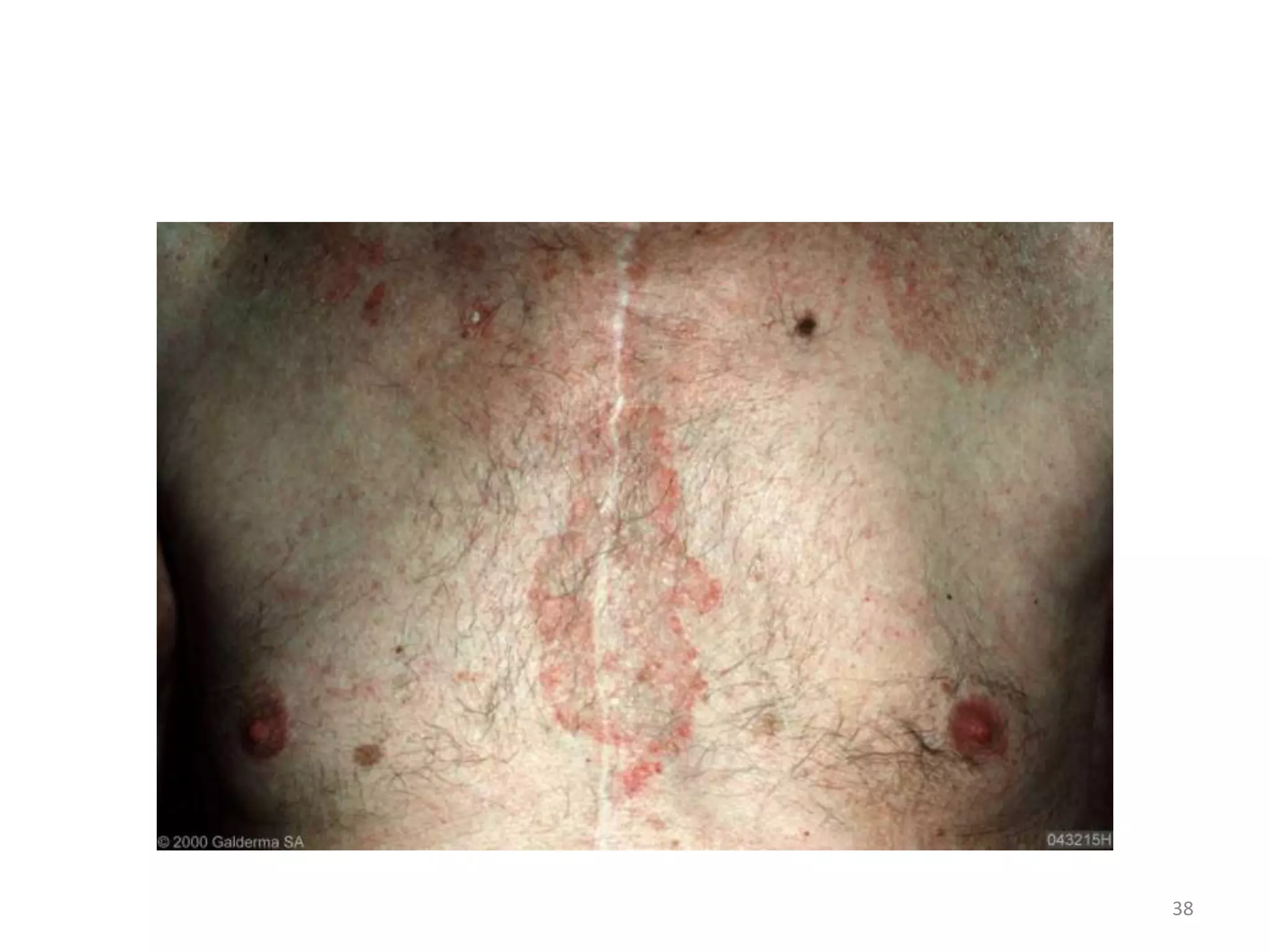
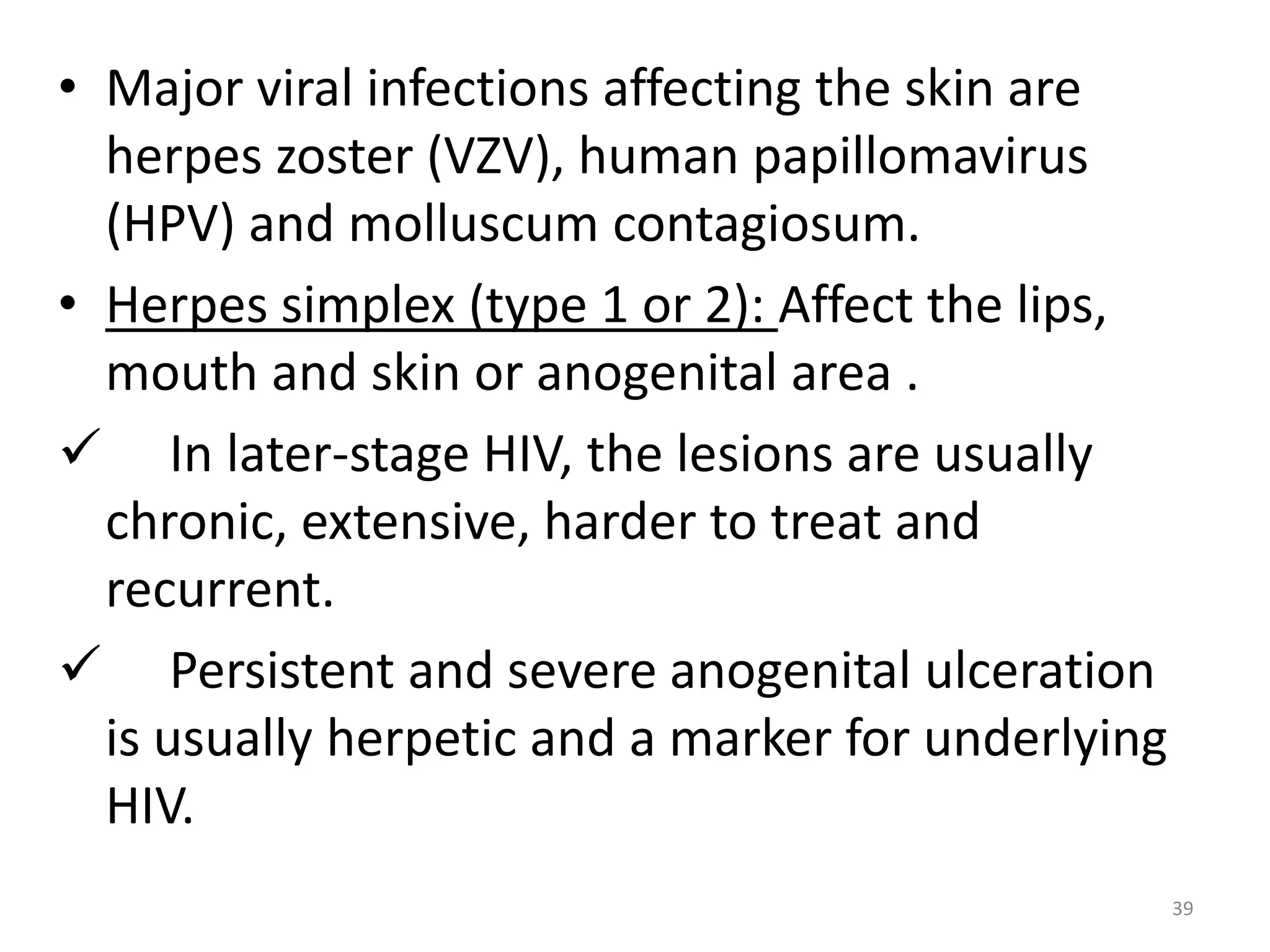
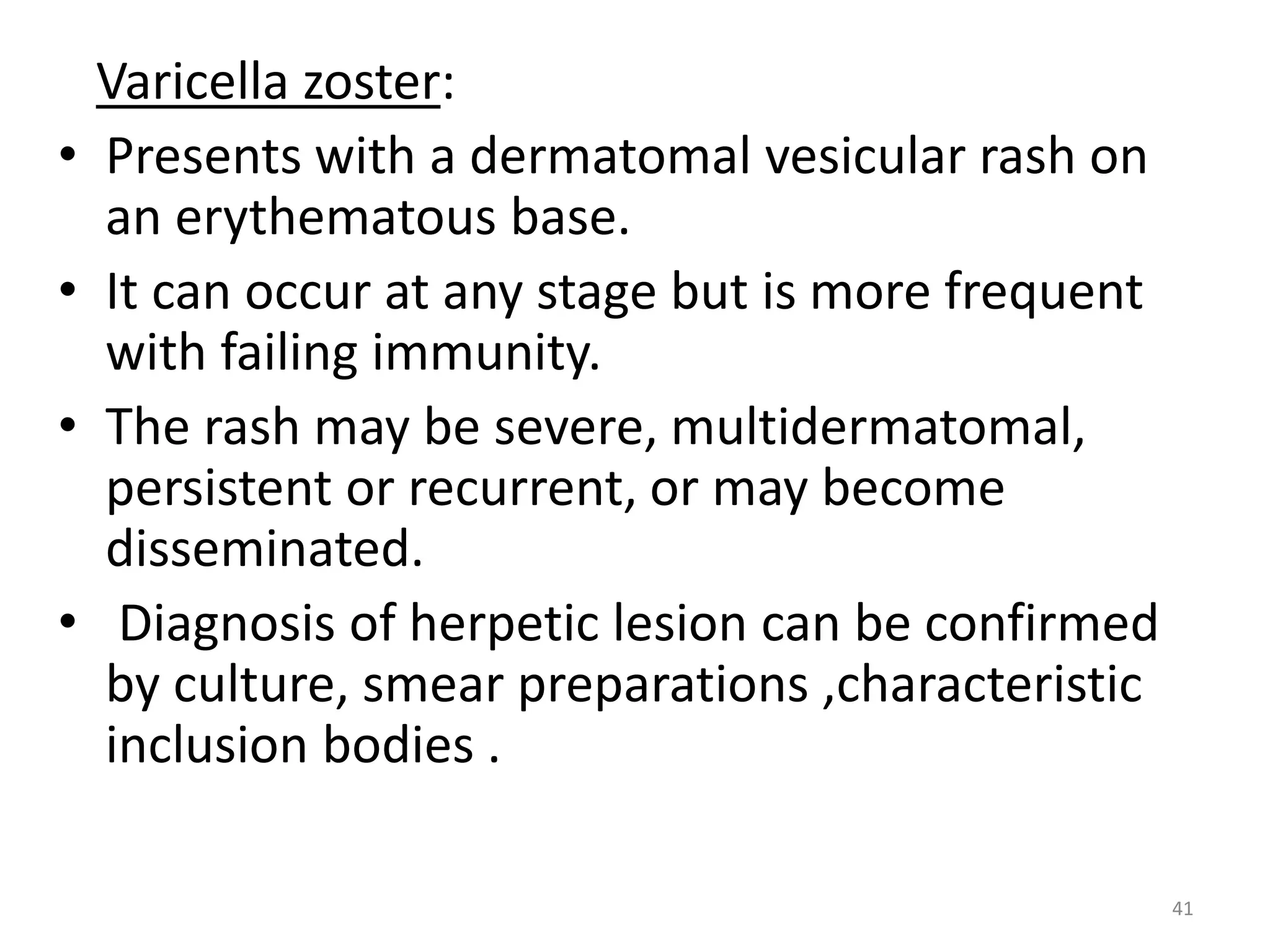
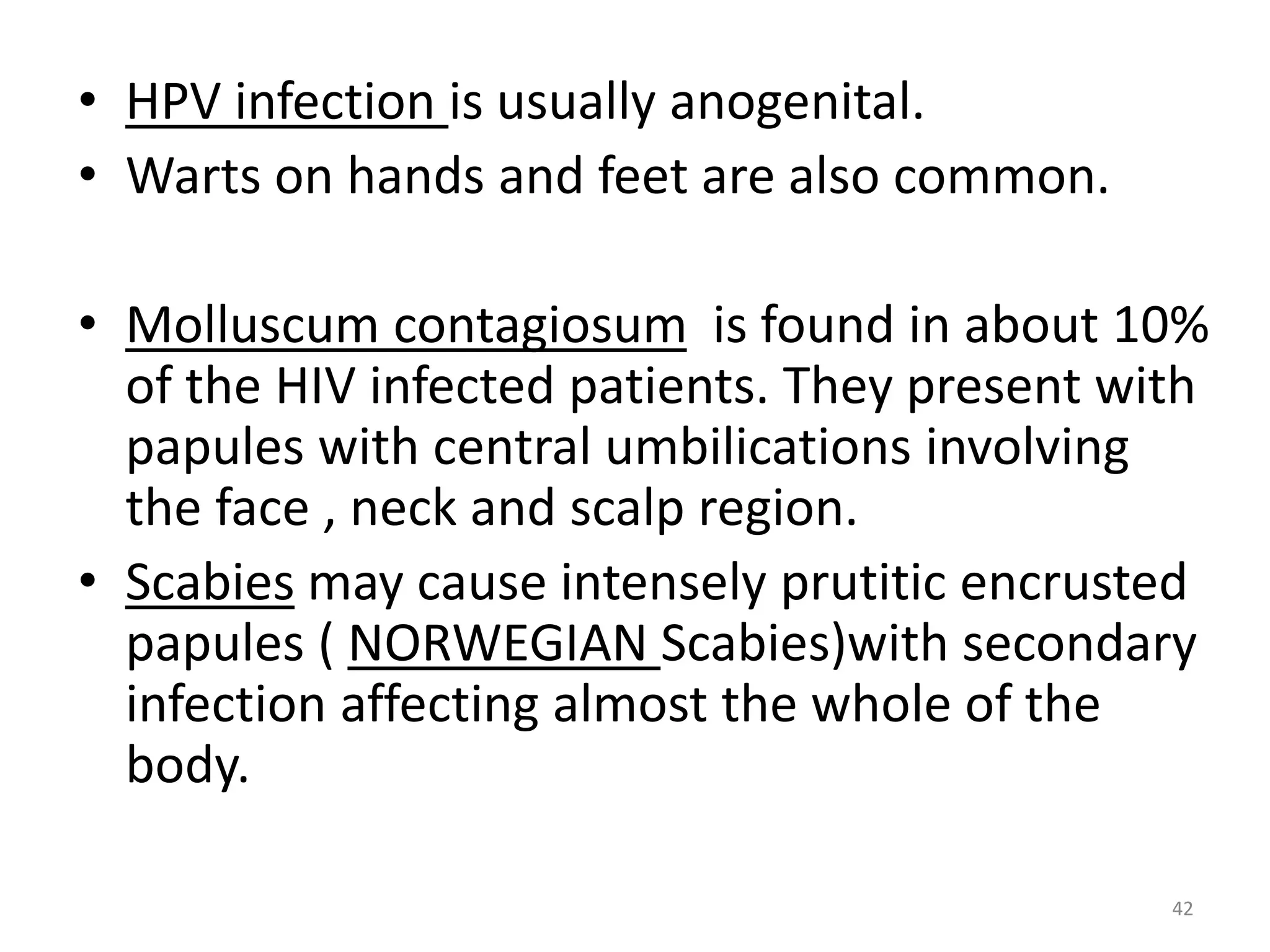
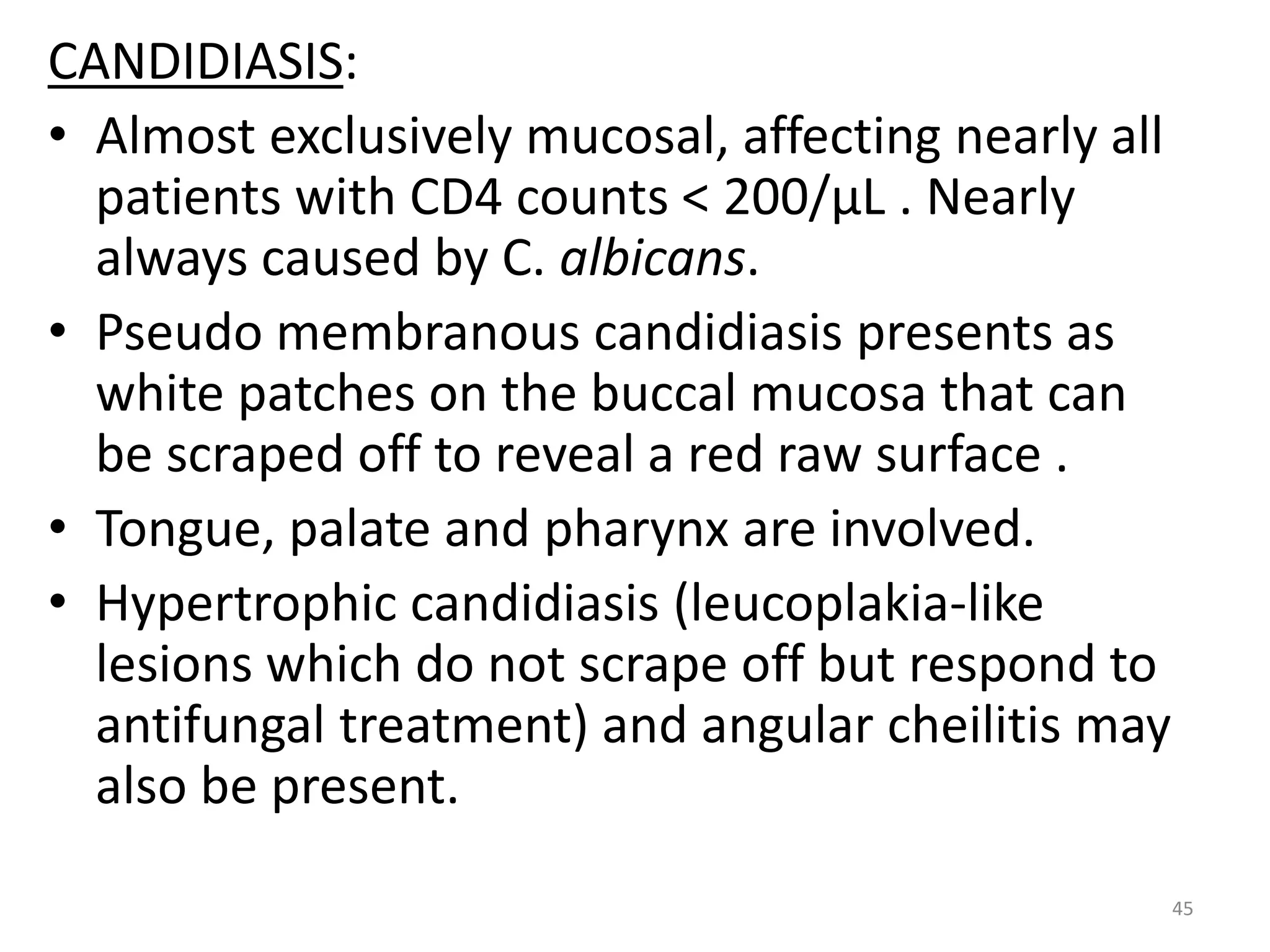
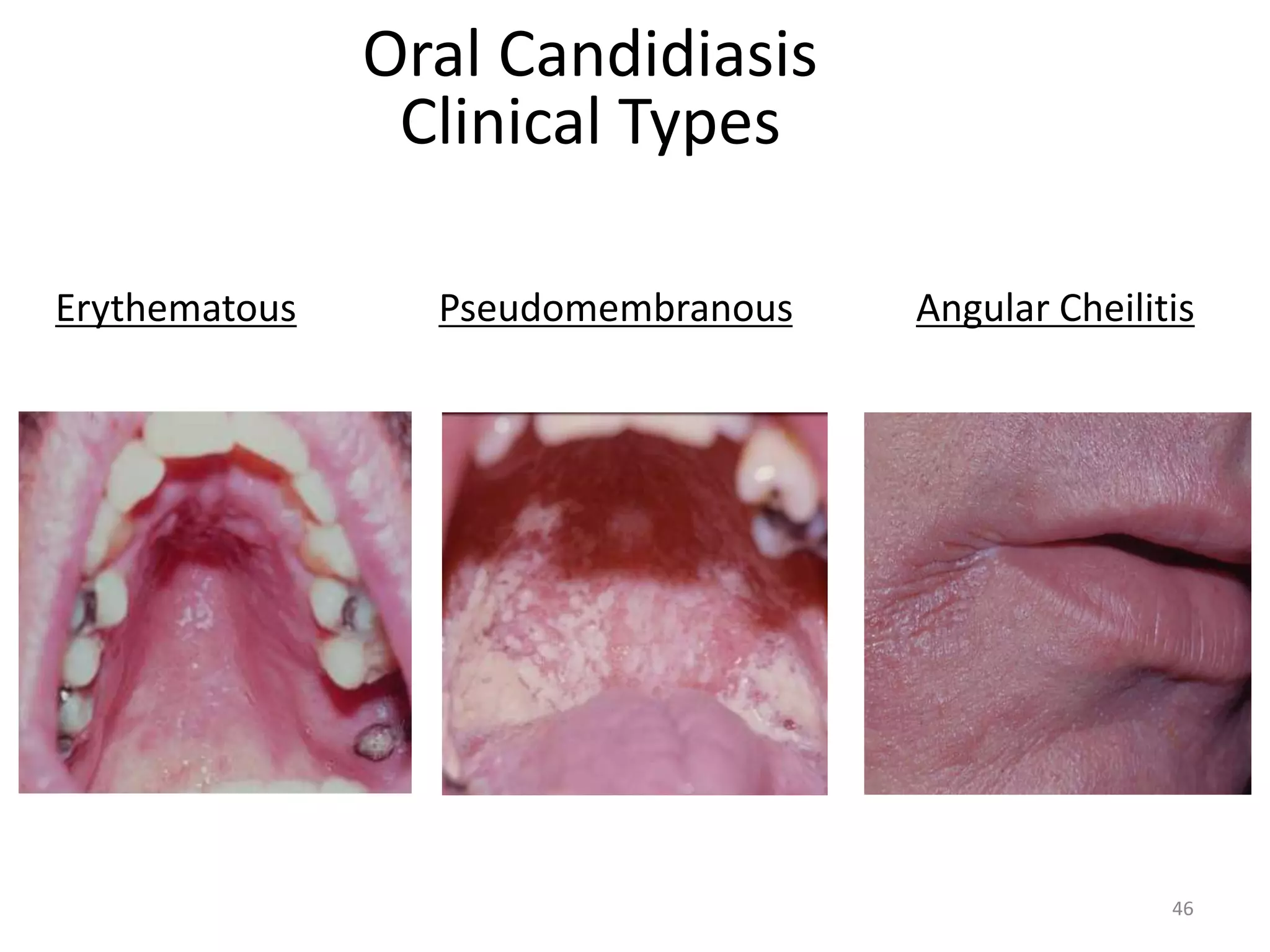
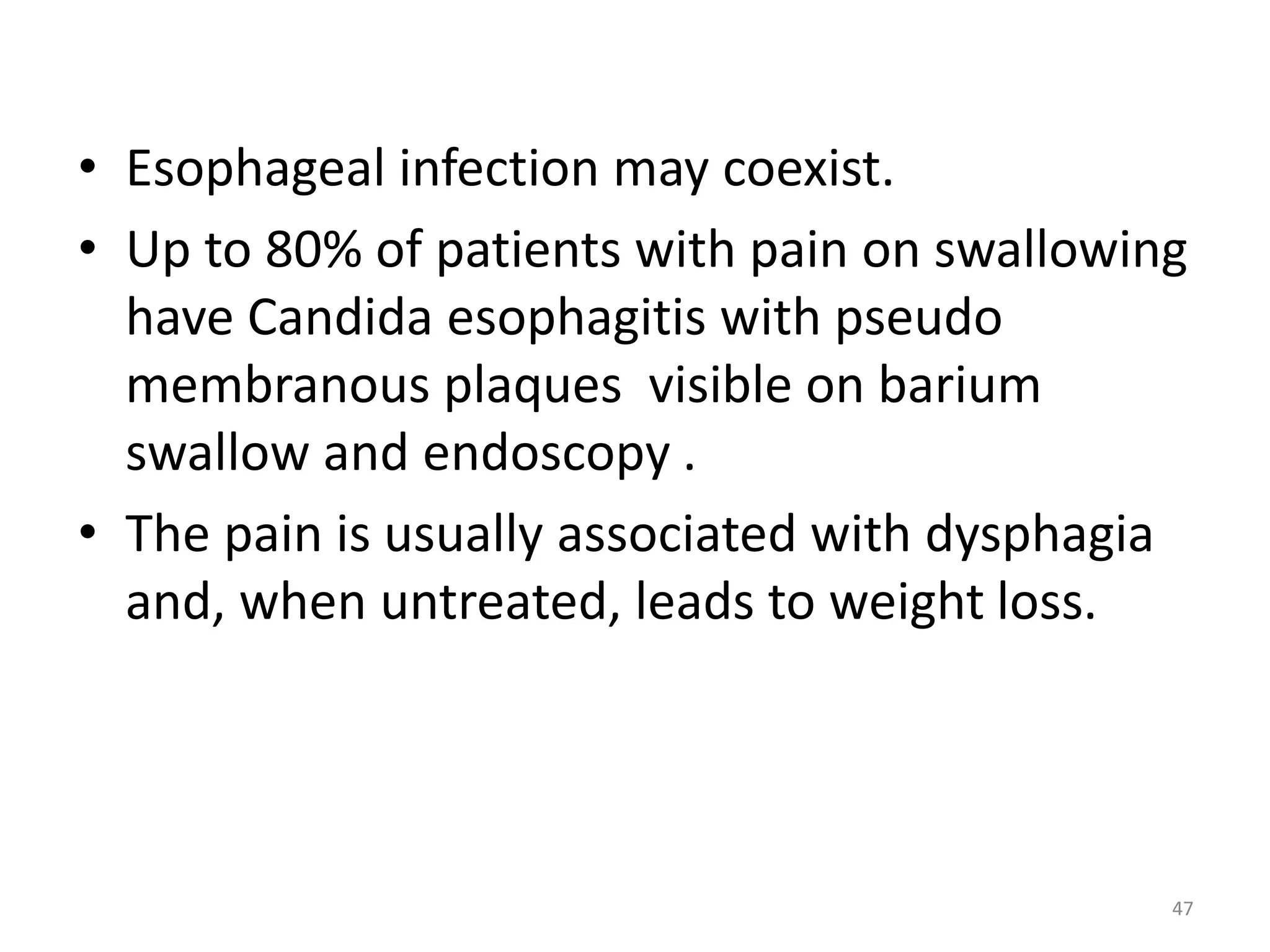
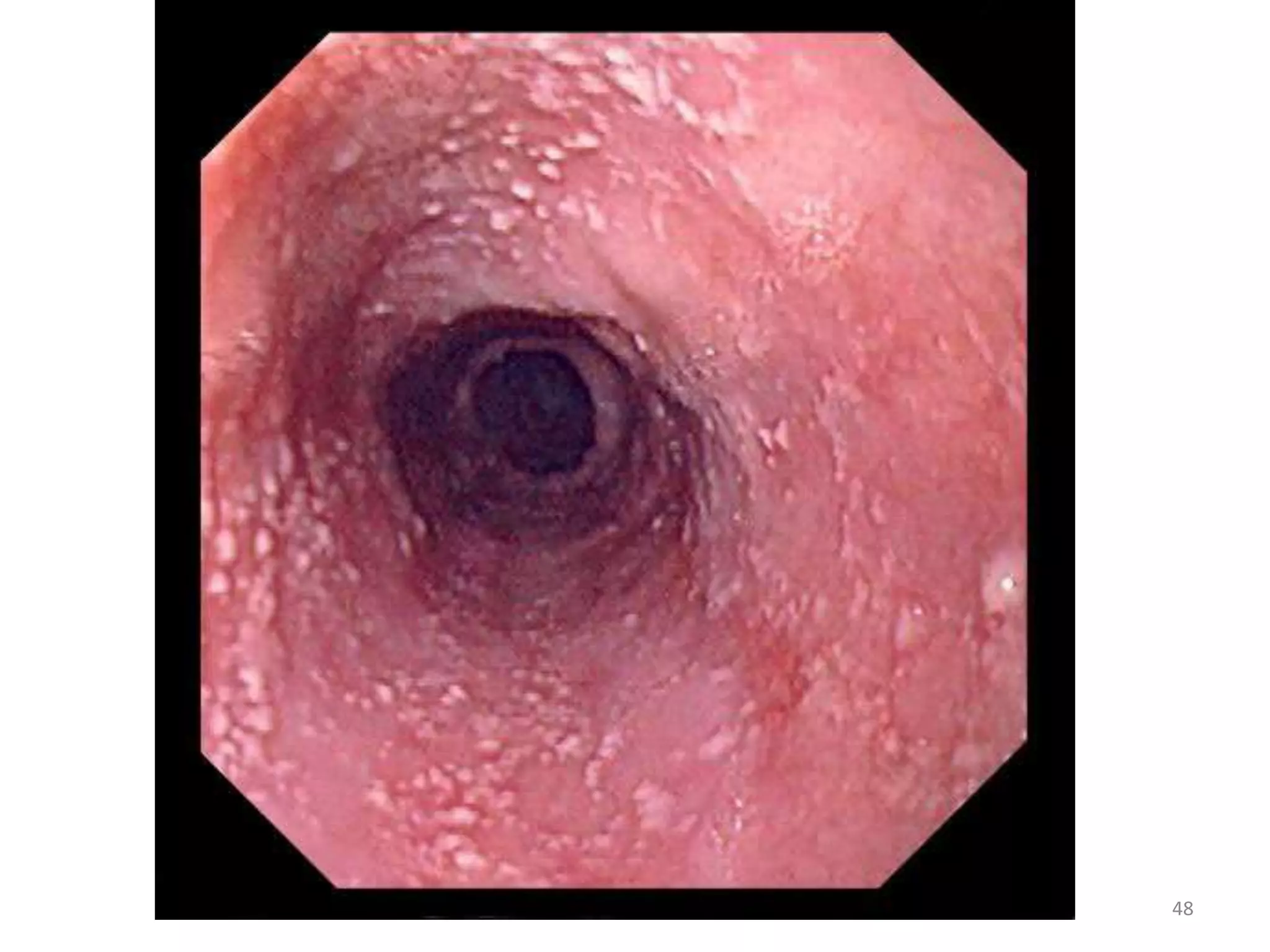
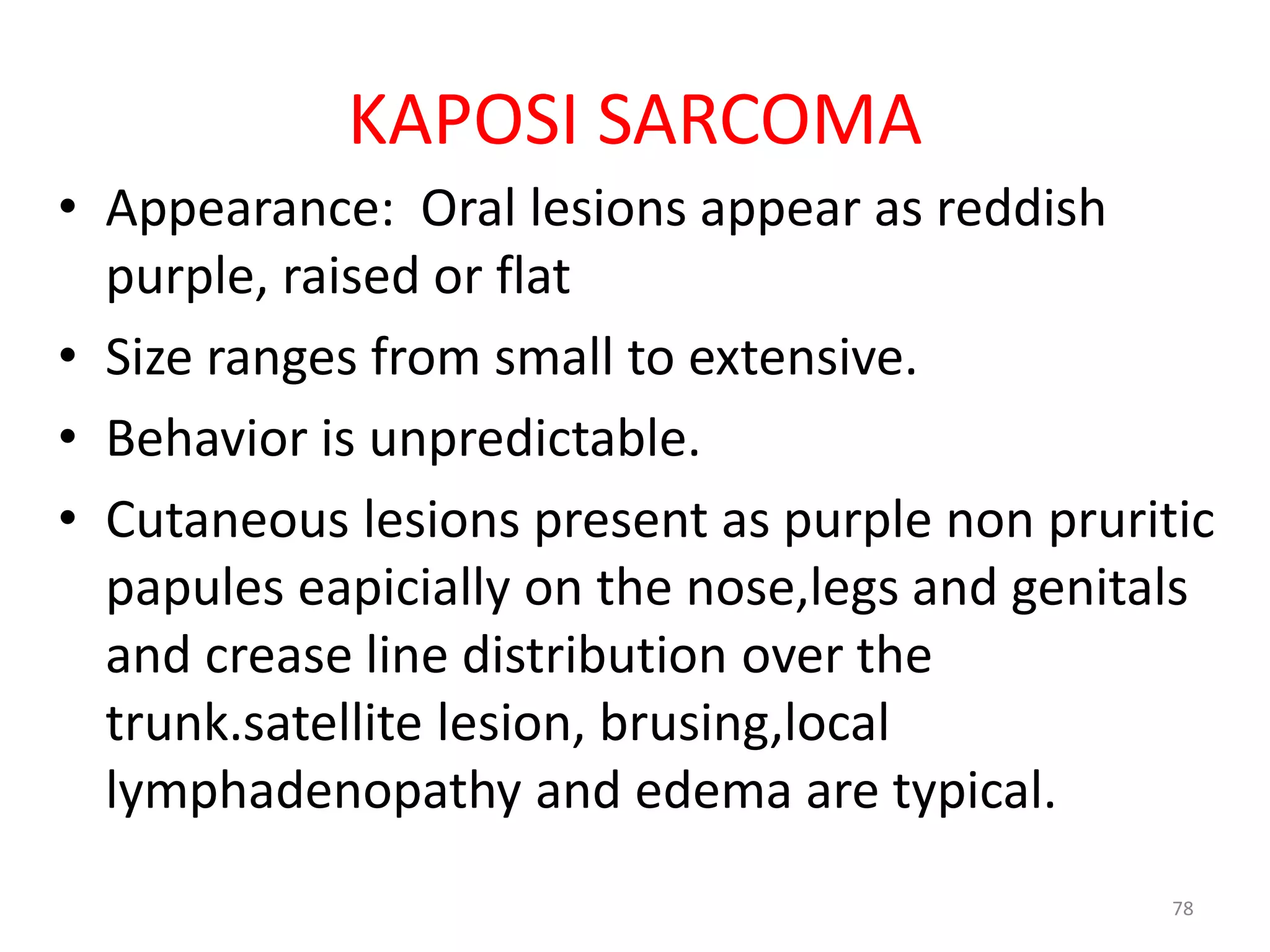
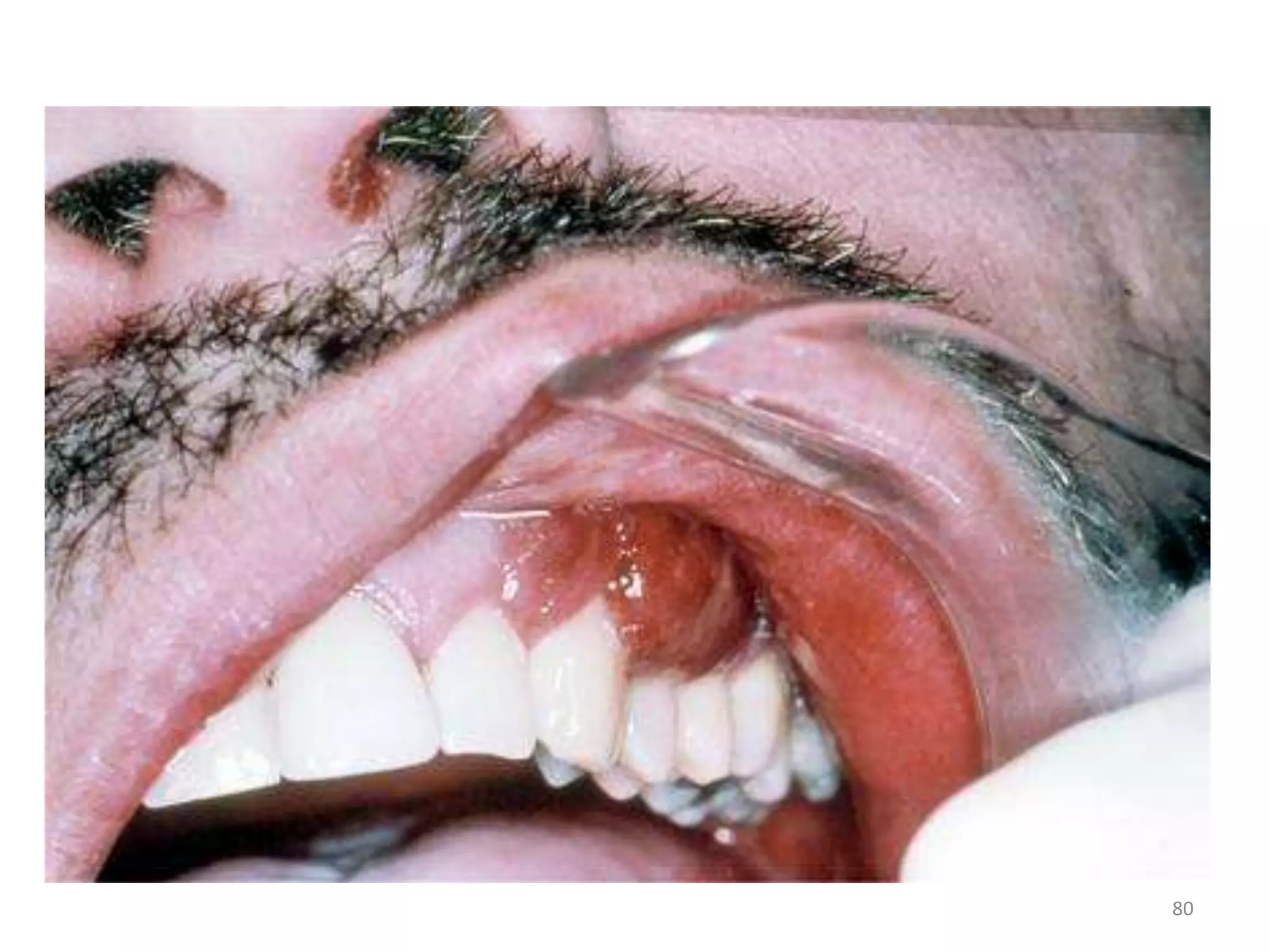
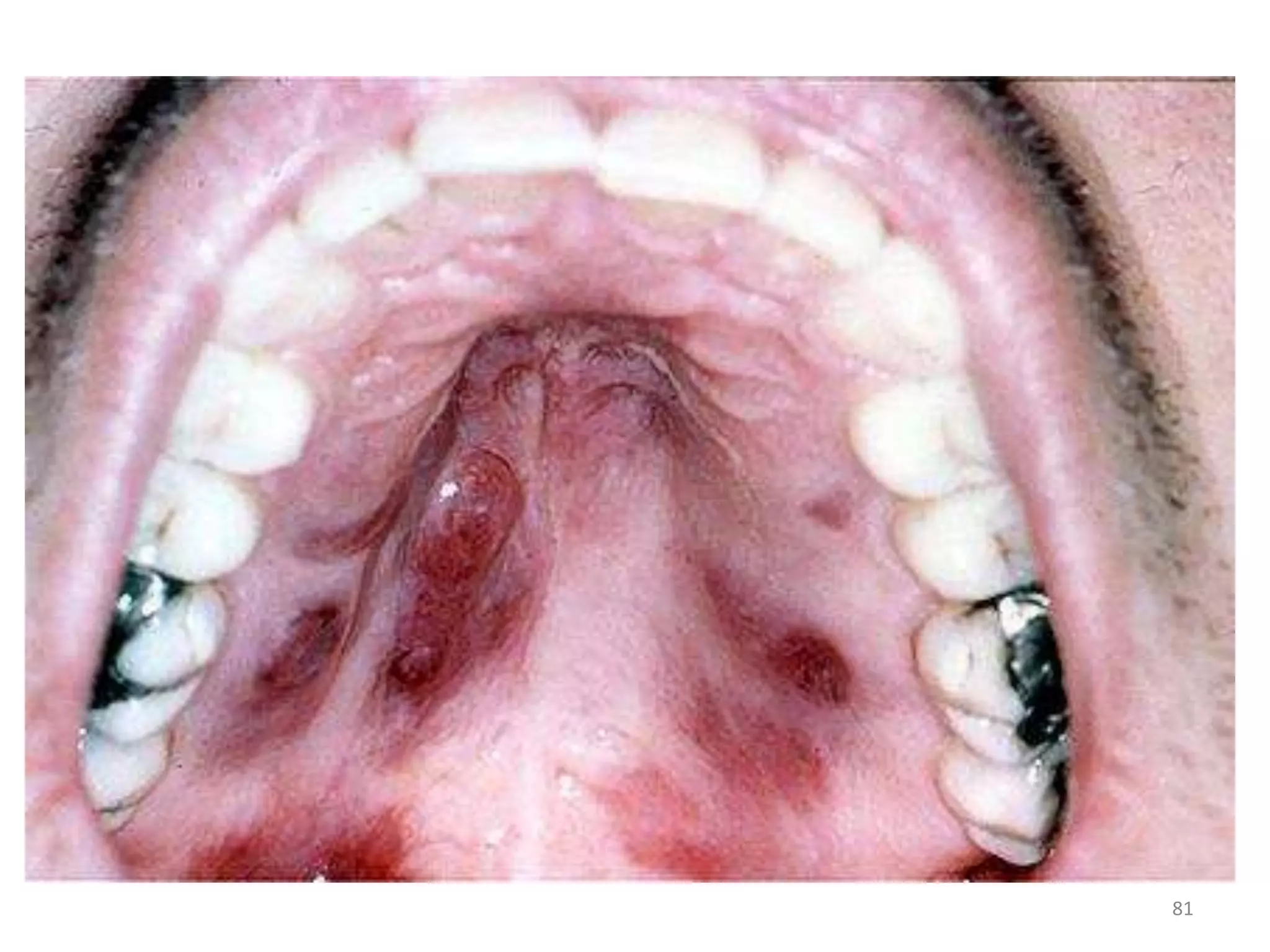
This document discusses the presenting problems in HIV infection. It describes the stages of infection from acute to asymptomatic to symptomatic disease. Common respiratory infections associated with HIV include pneumonia, Pneumocystis jiroveci pneumonia, tuberculosis, and atypical mycobacterial infections. Other organ systems affected by opportunistic infections in HIV patients with low CD4 counts include the cardiovascular and gastrointestinal systems. Mucocutaneous manifestations are also common.