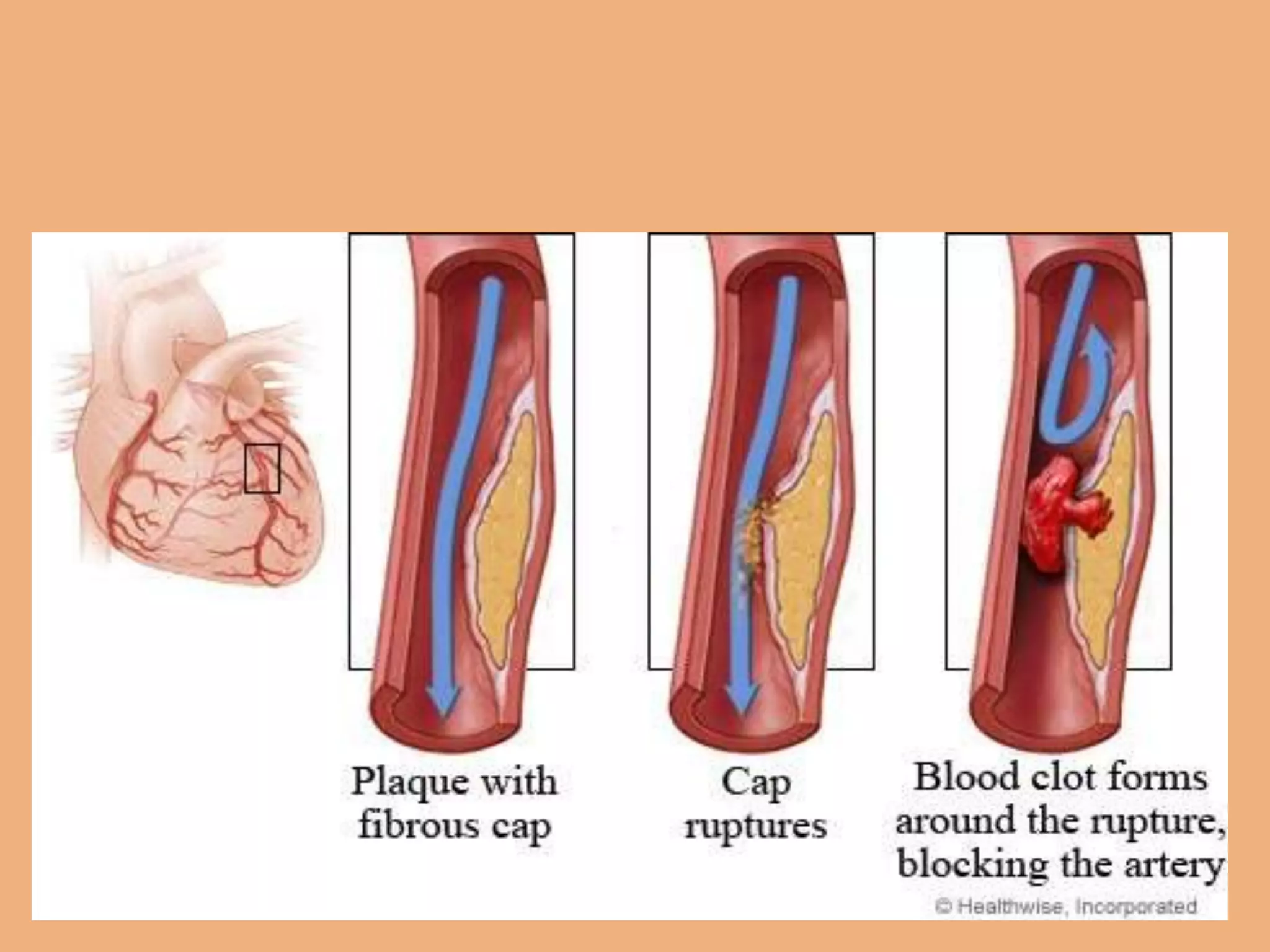
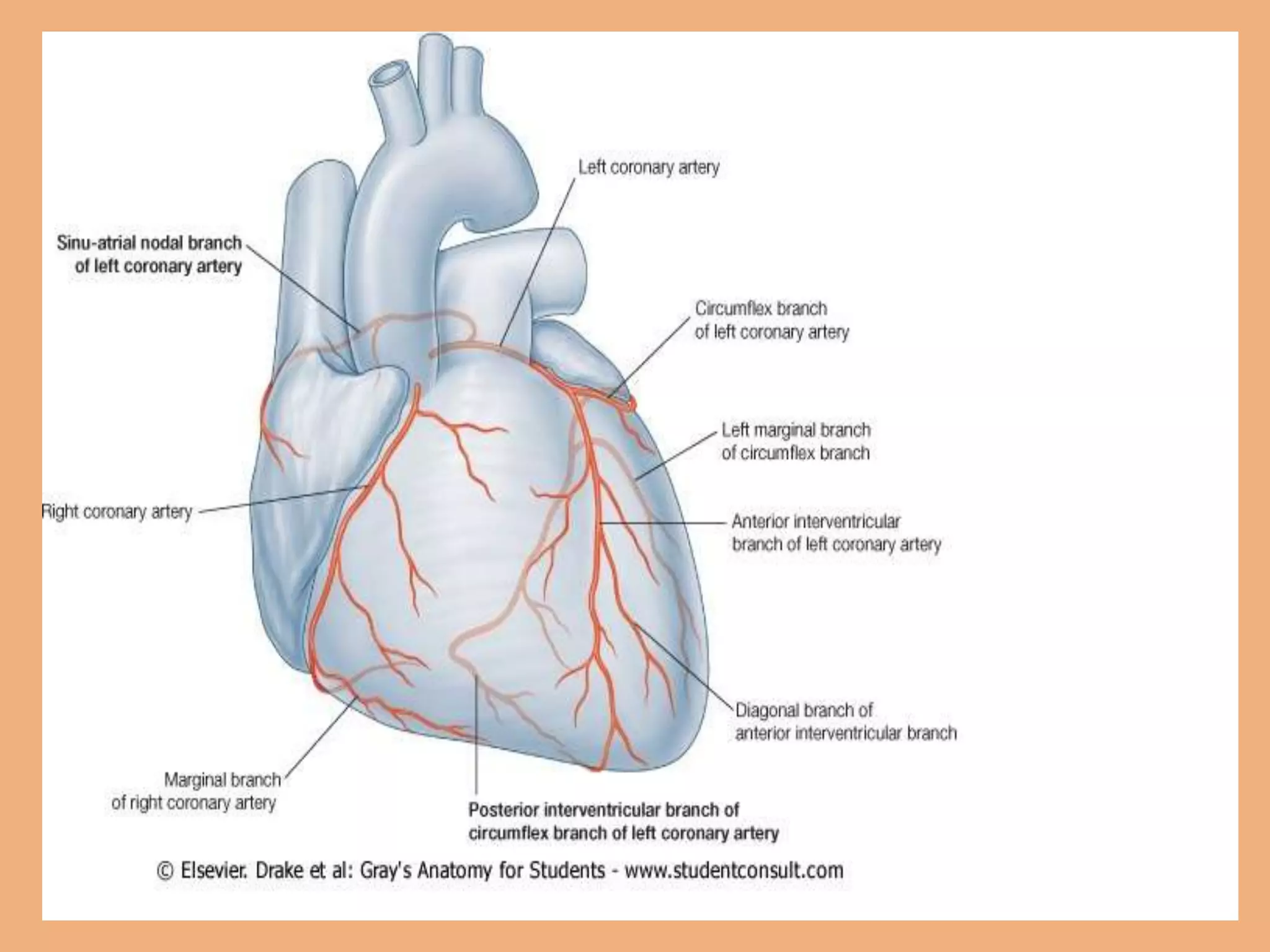
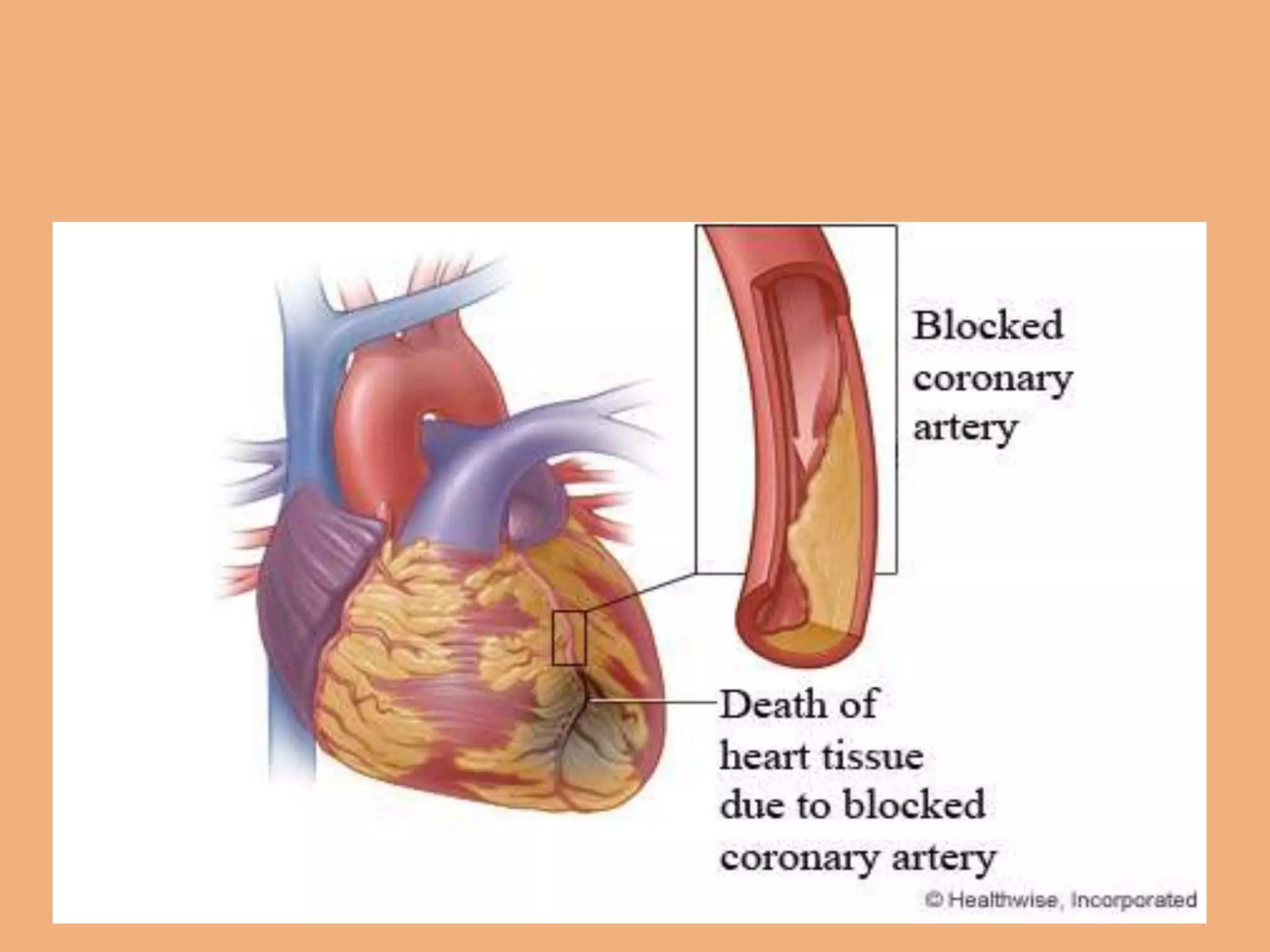
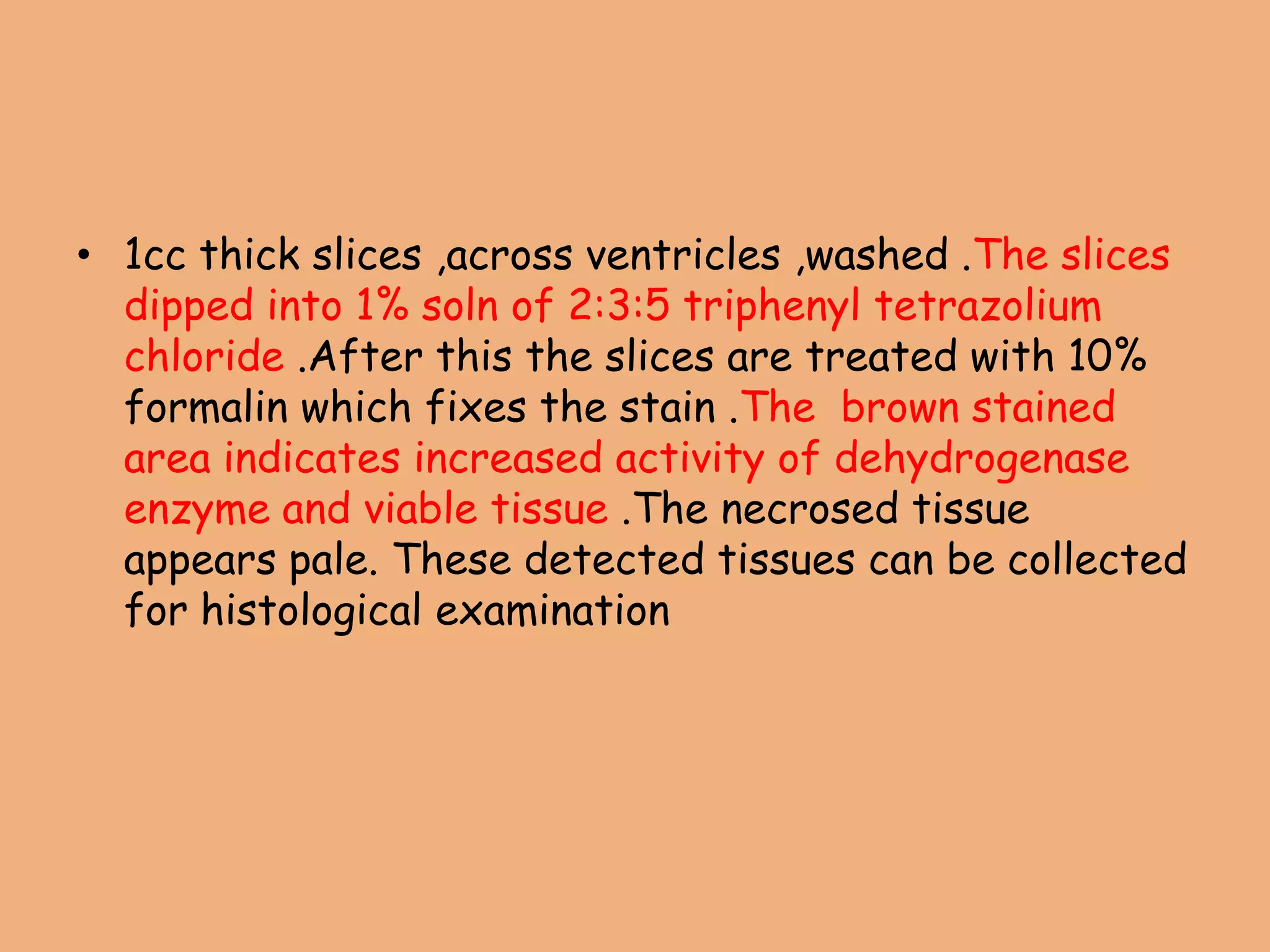
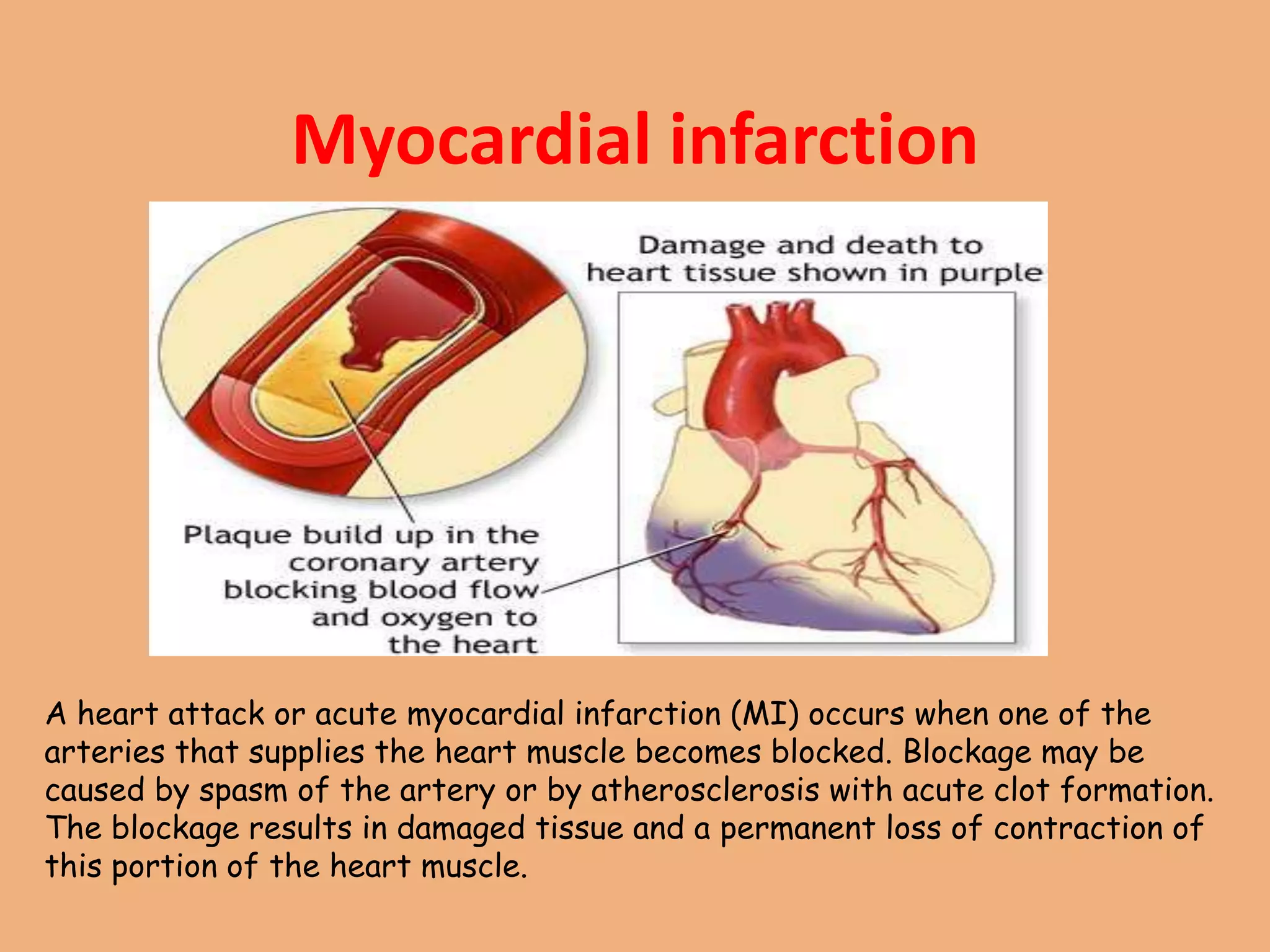
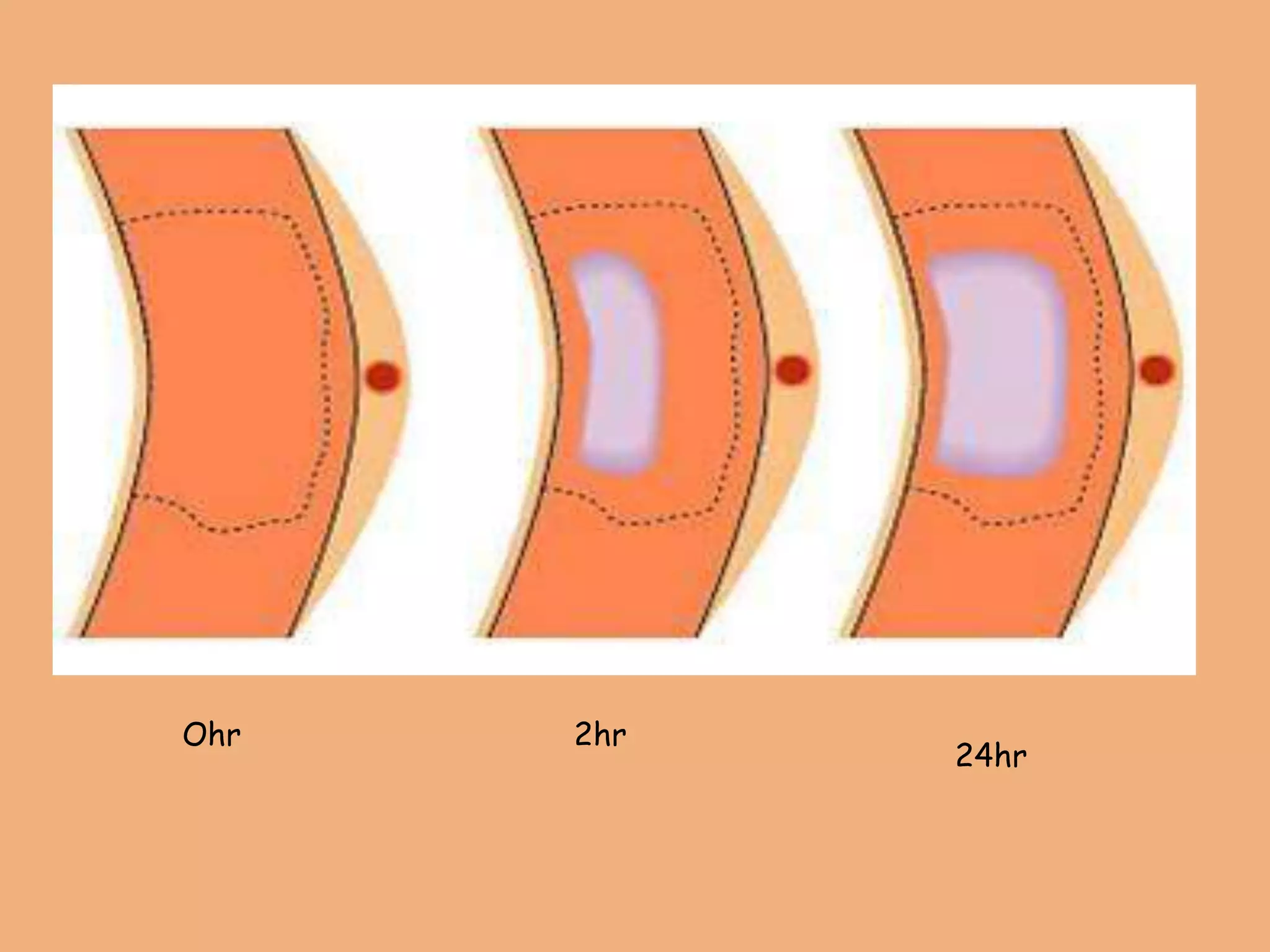
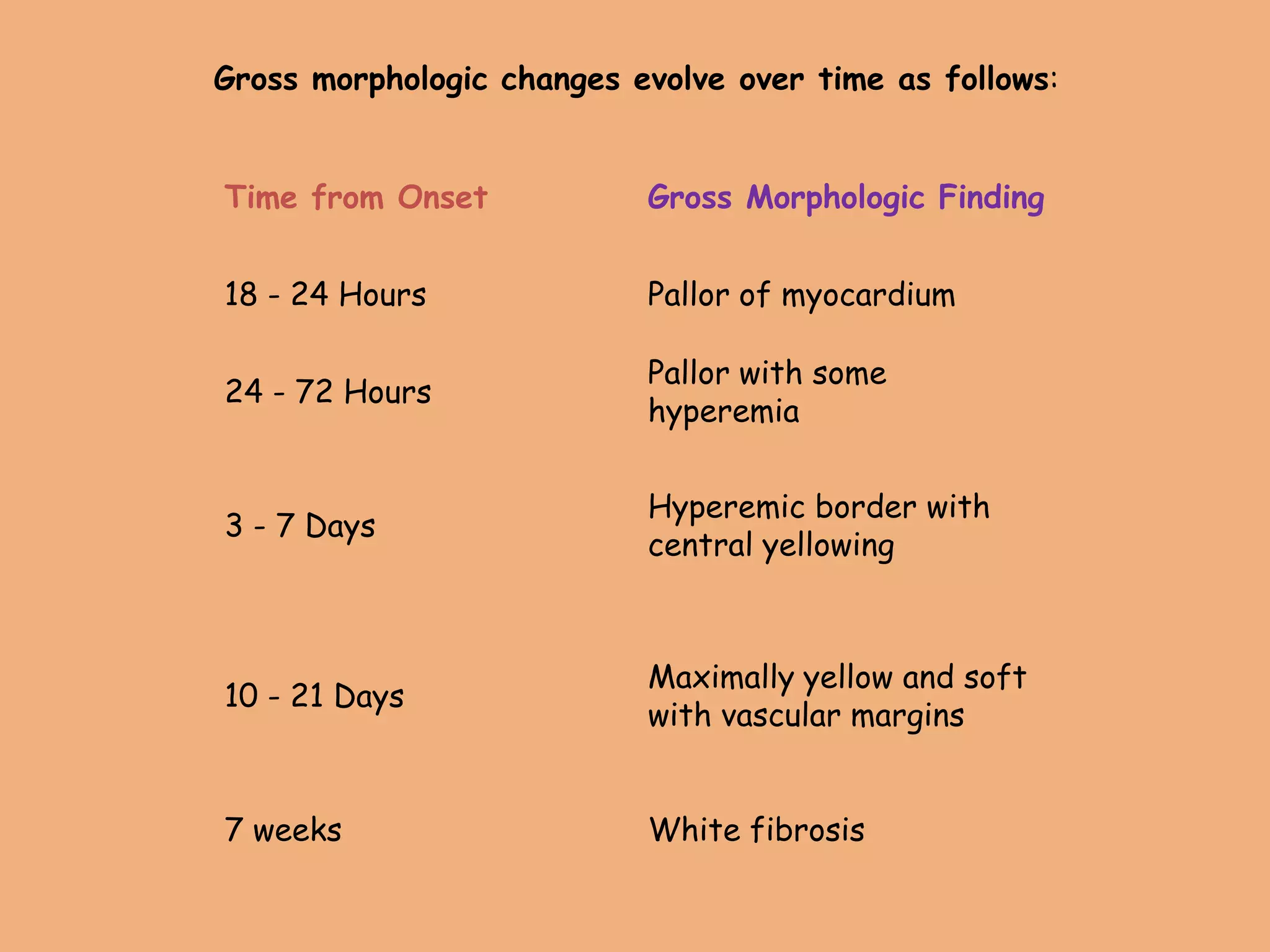
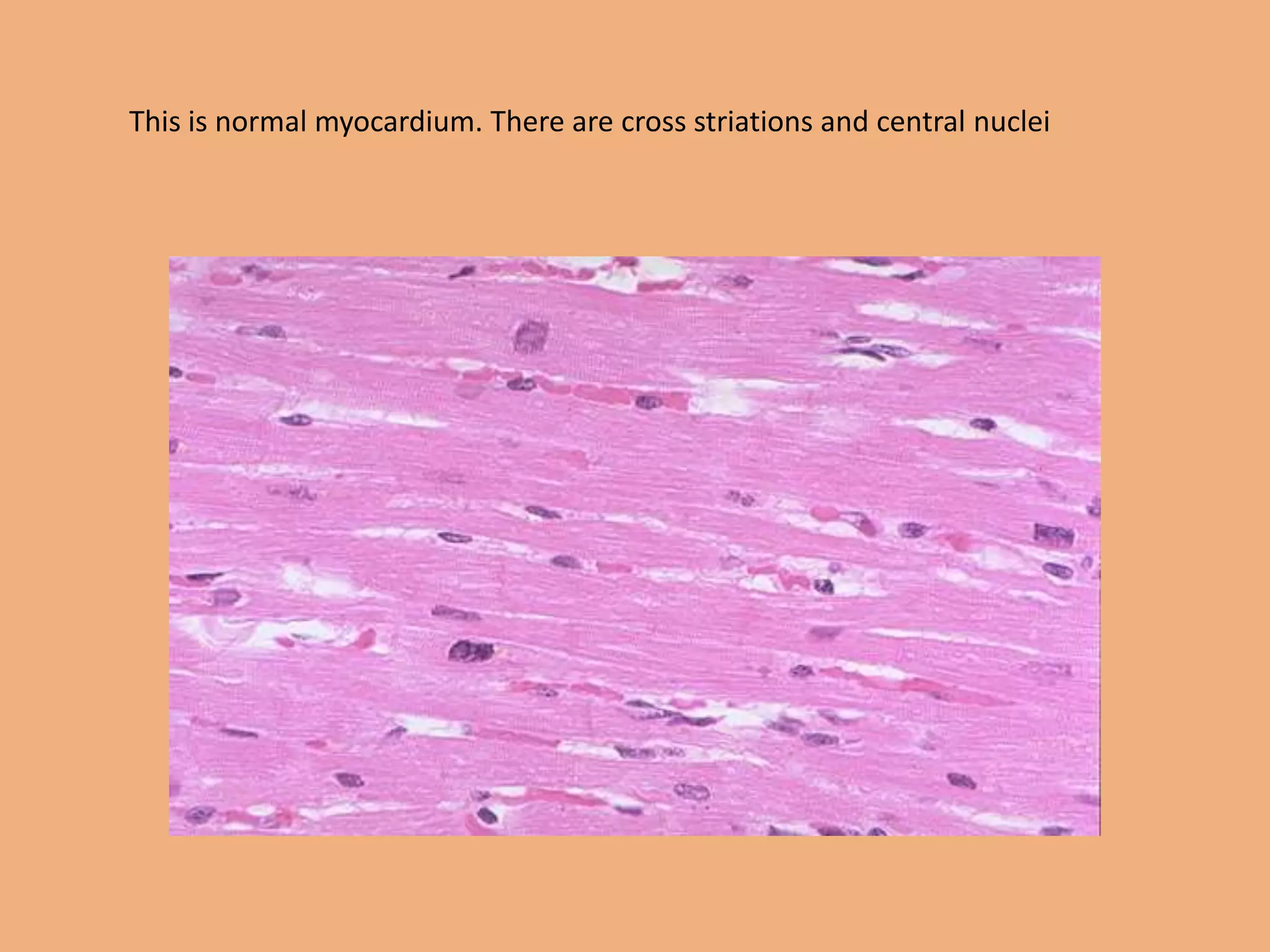
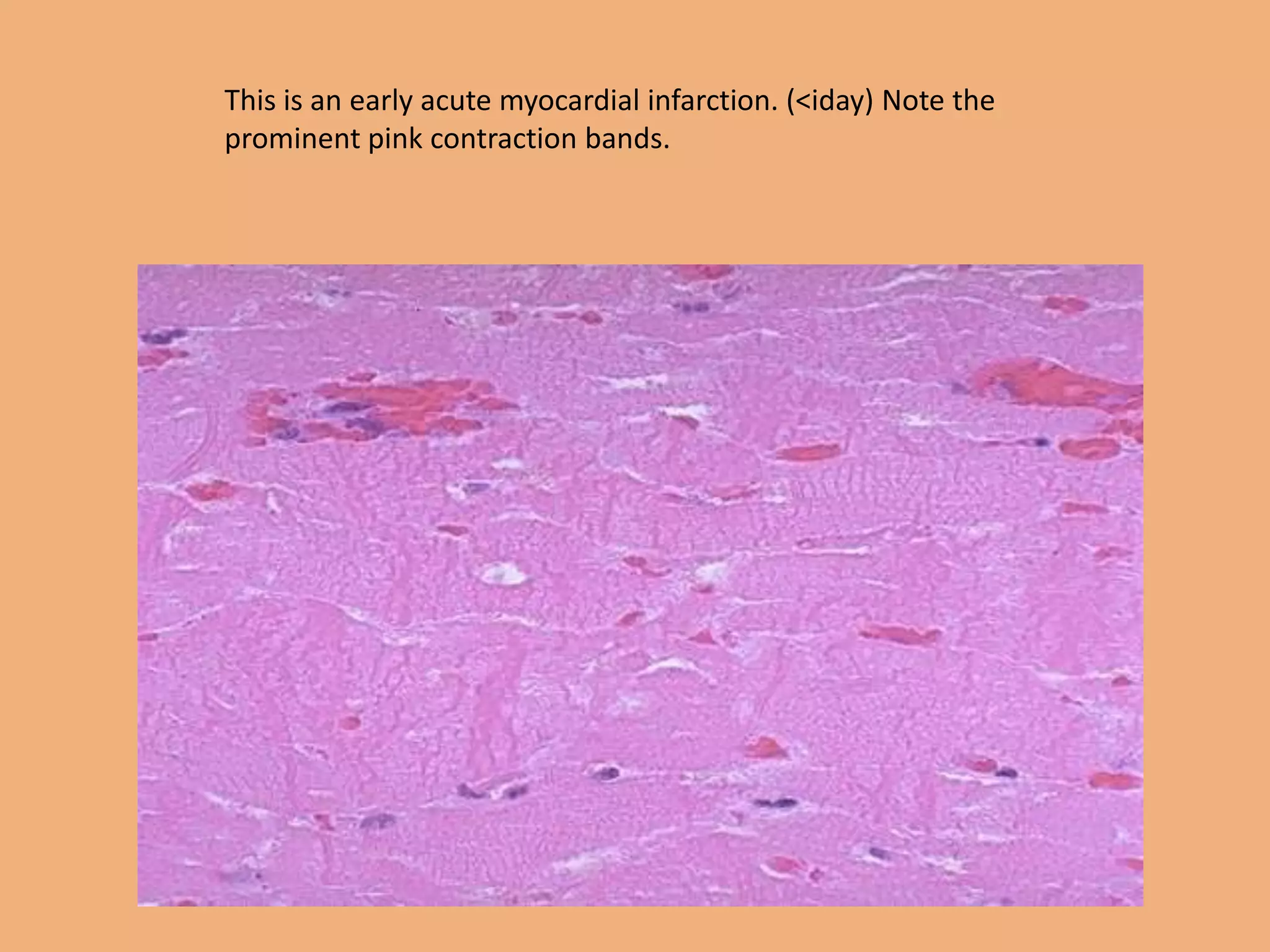
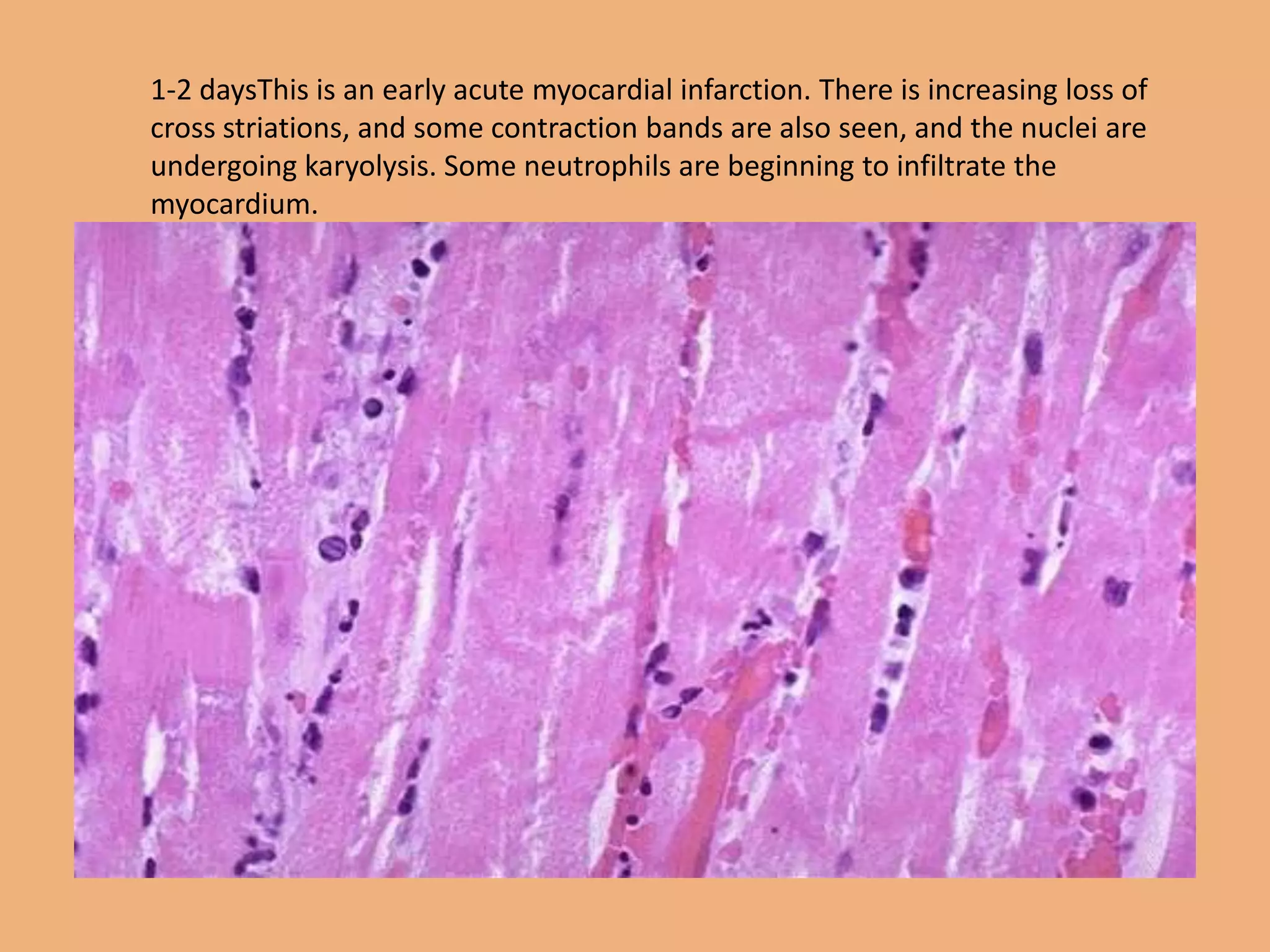
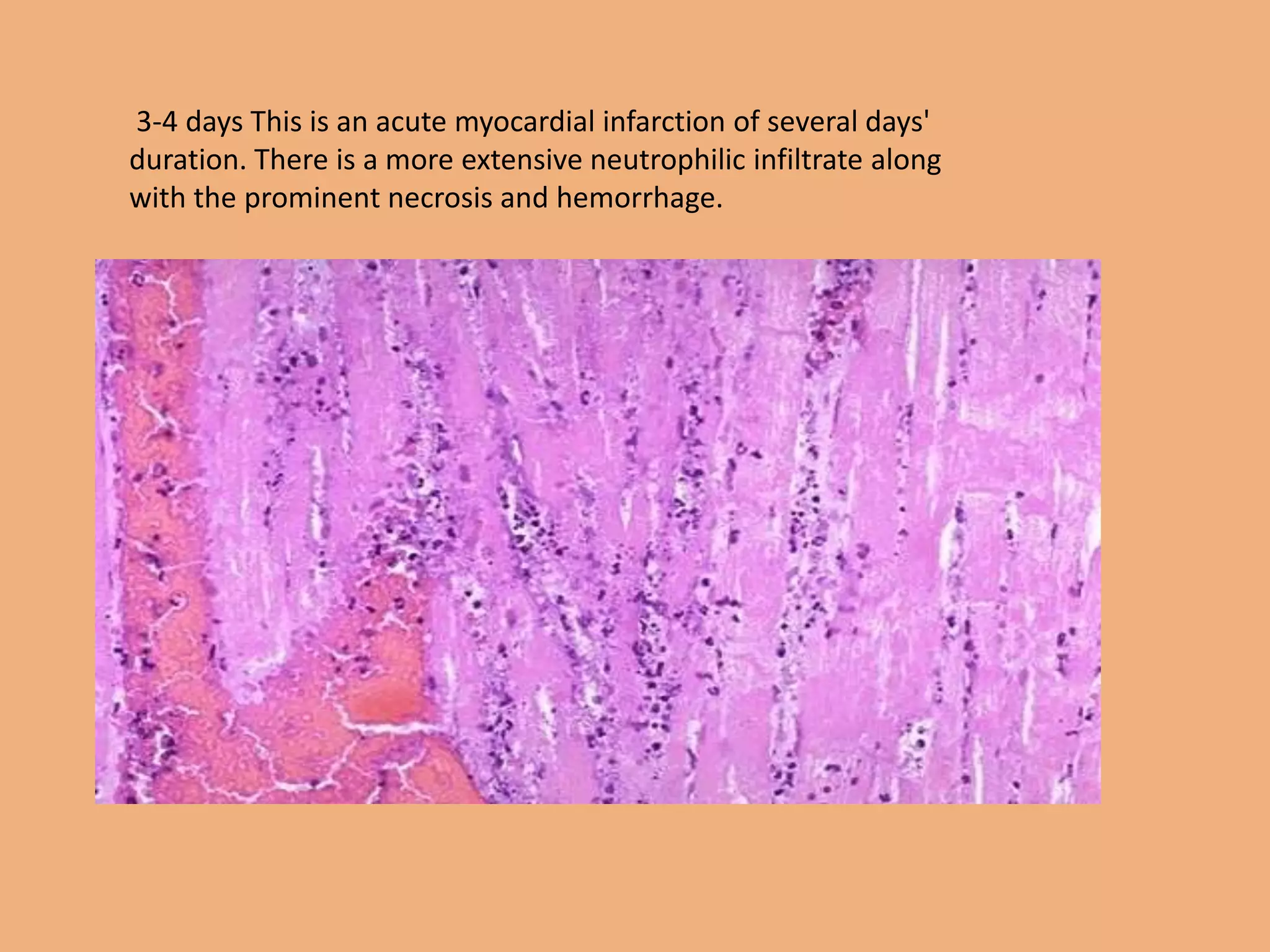
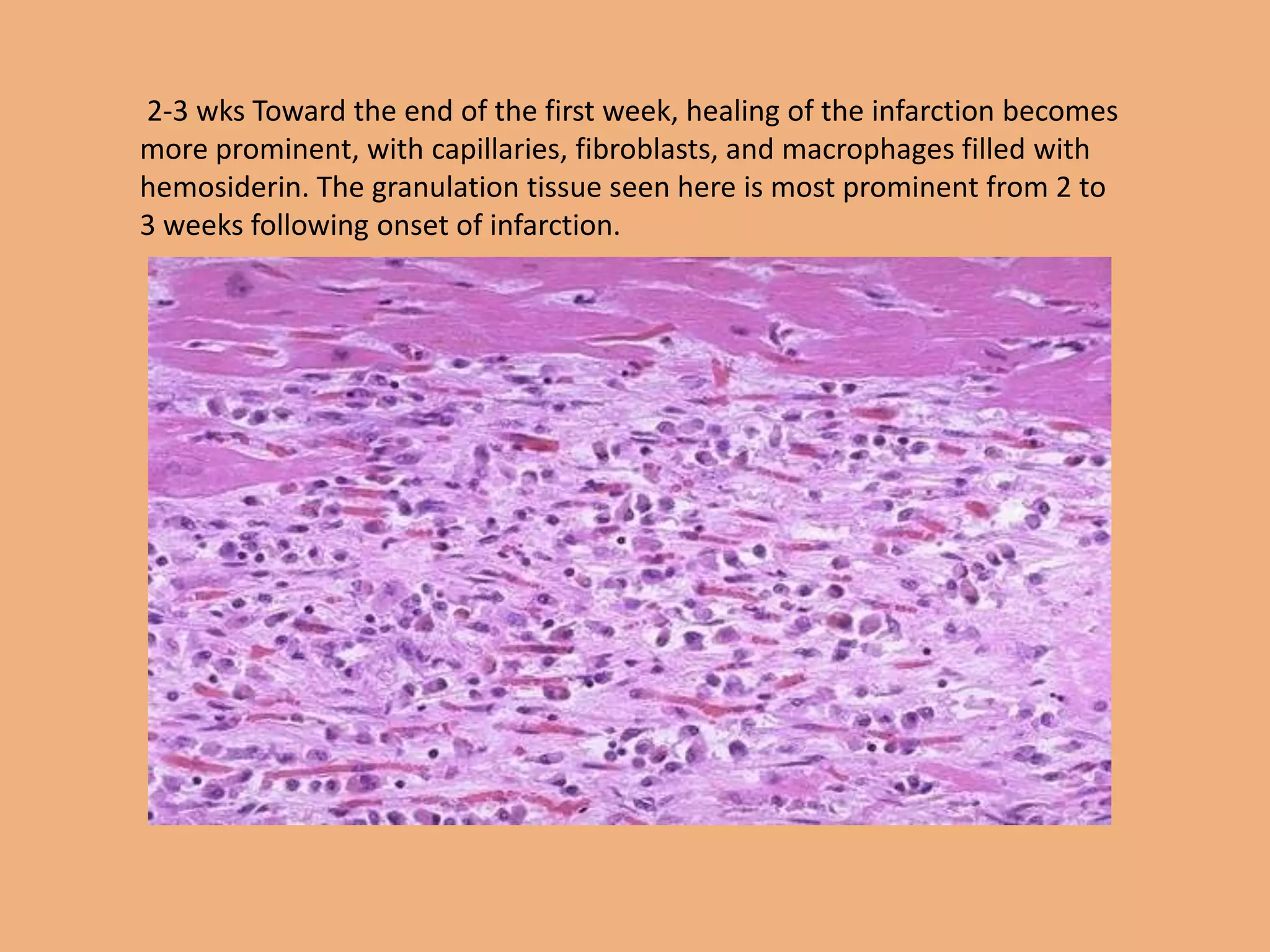
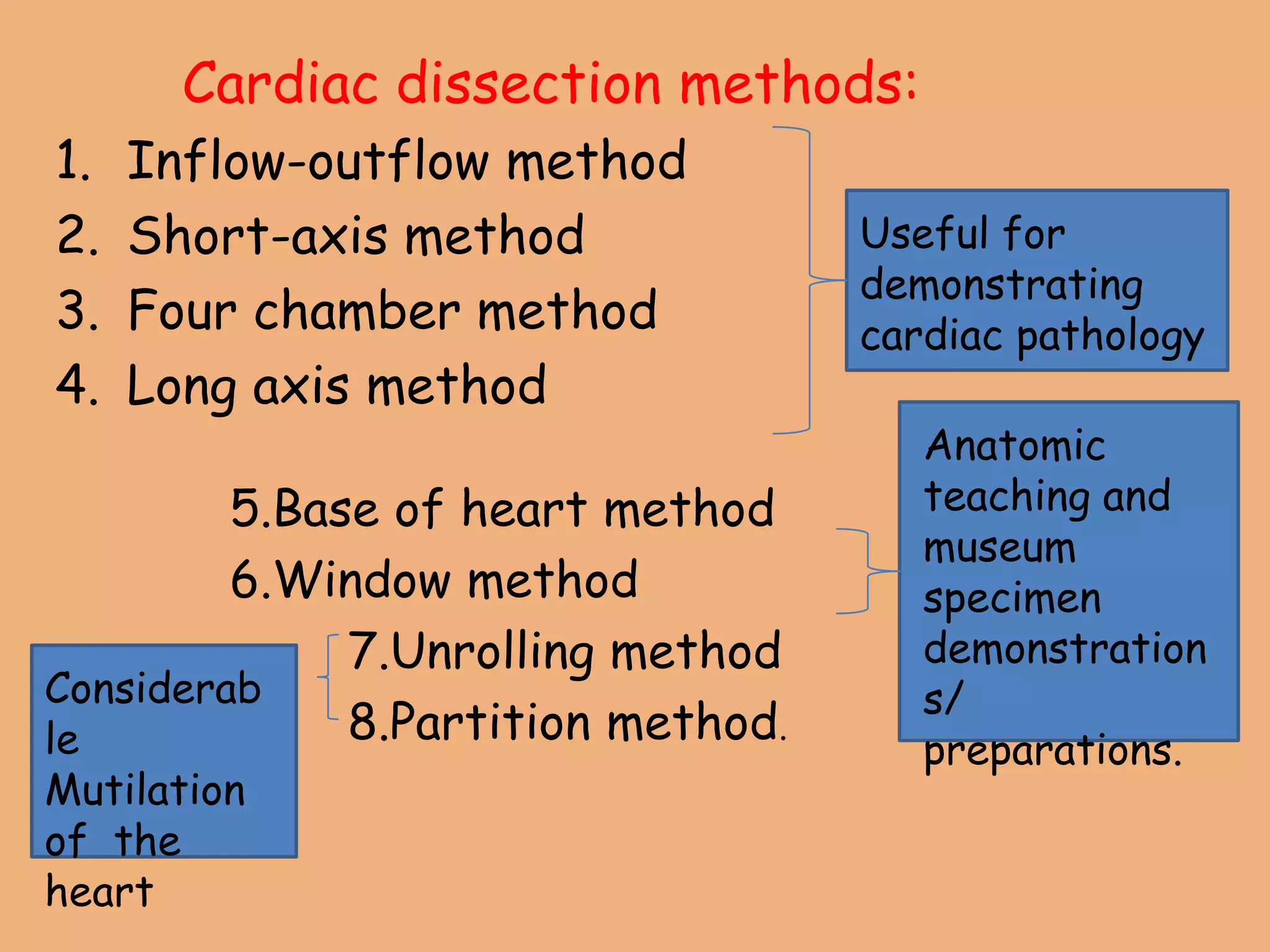
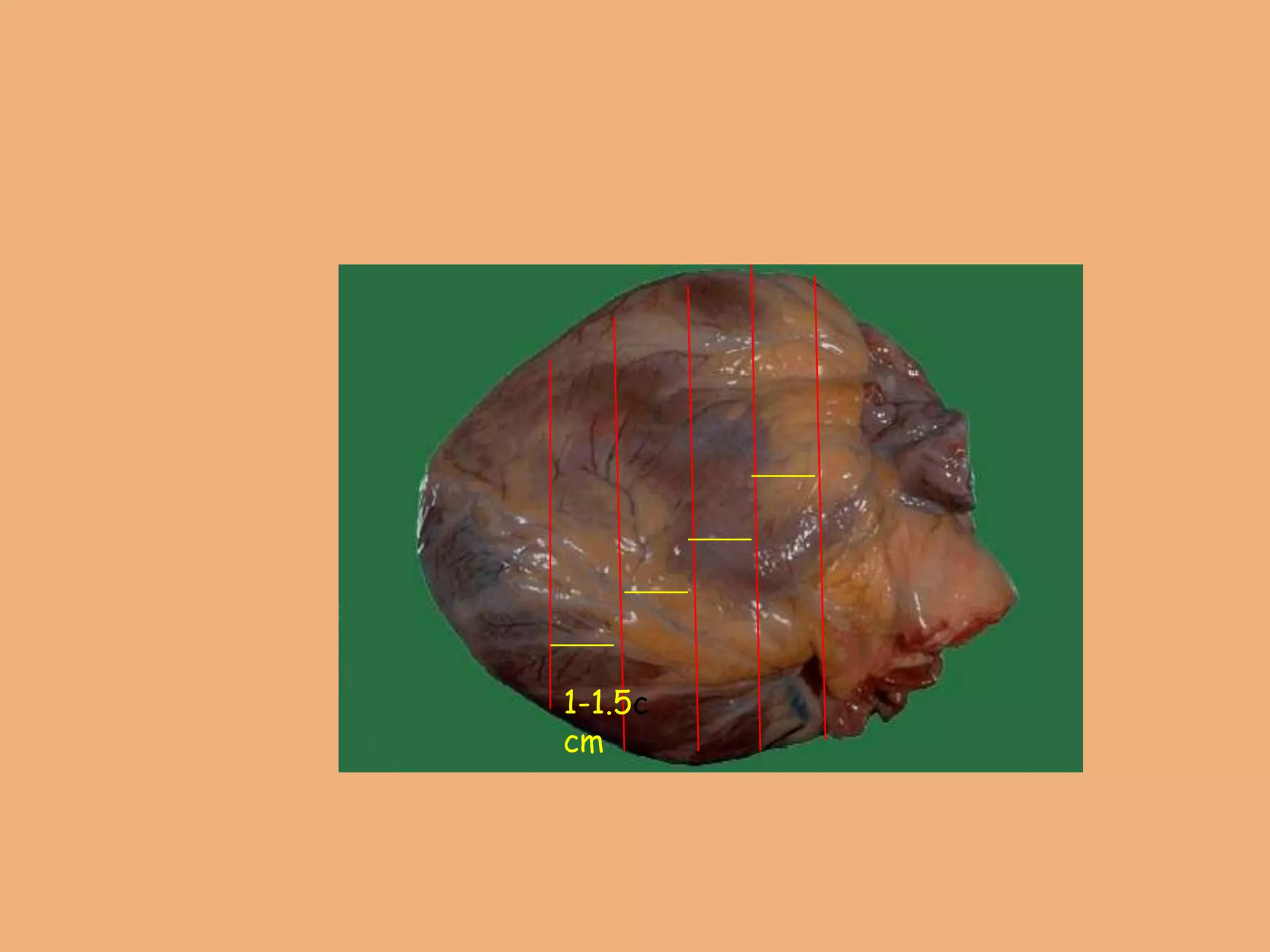
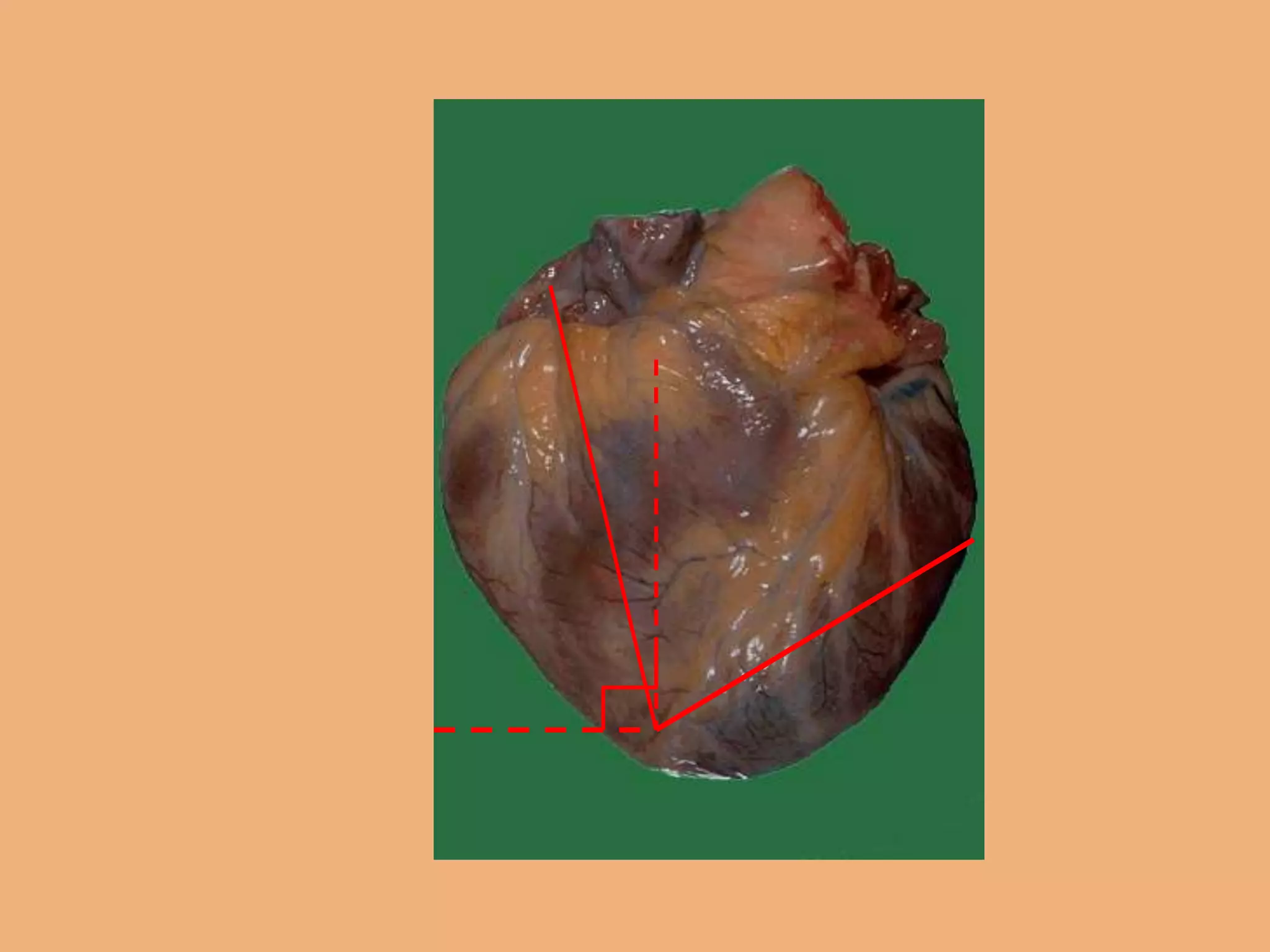
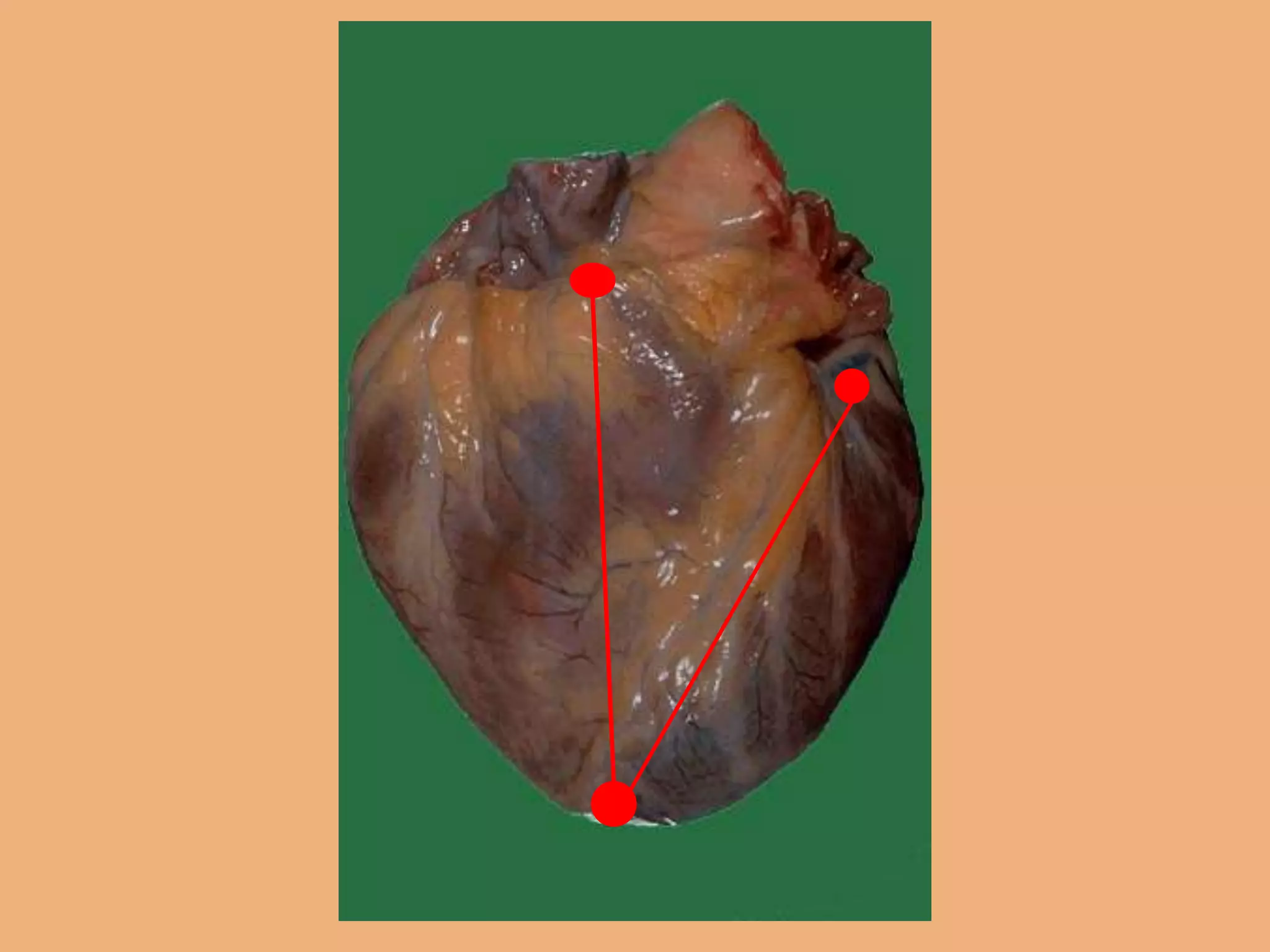
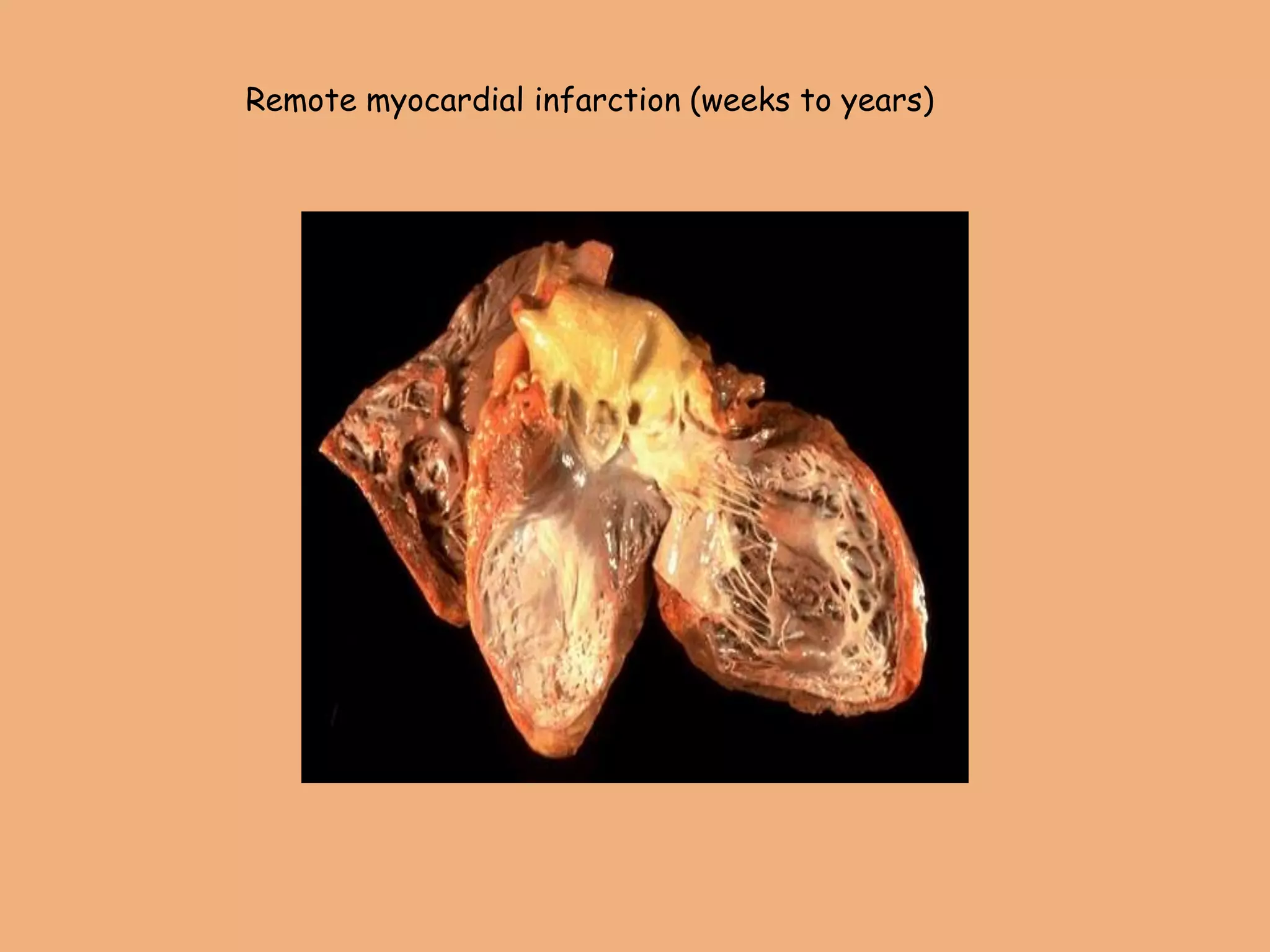
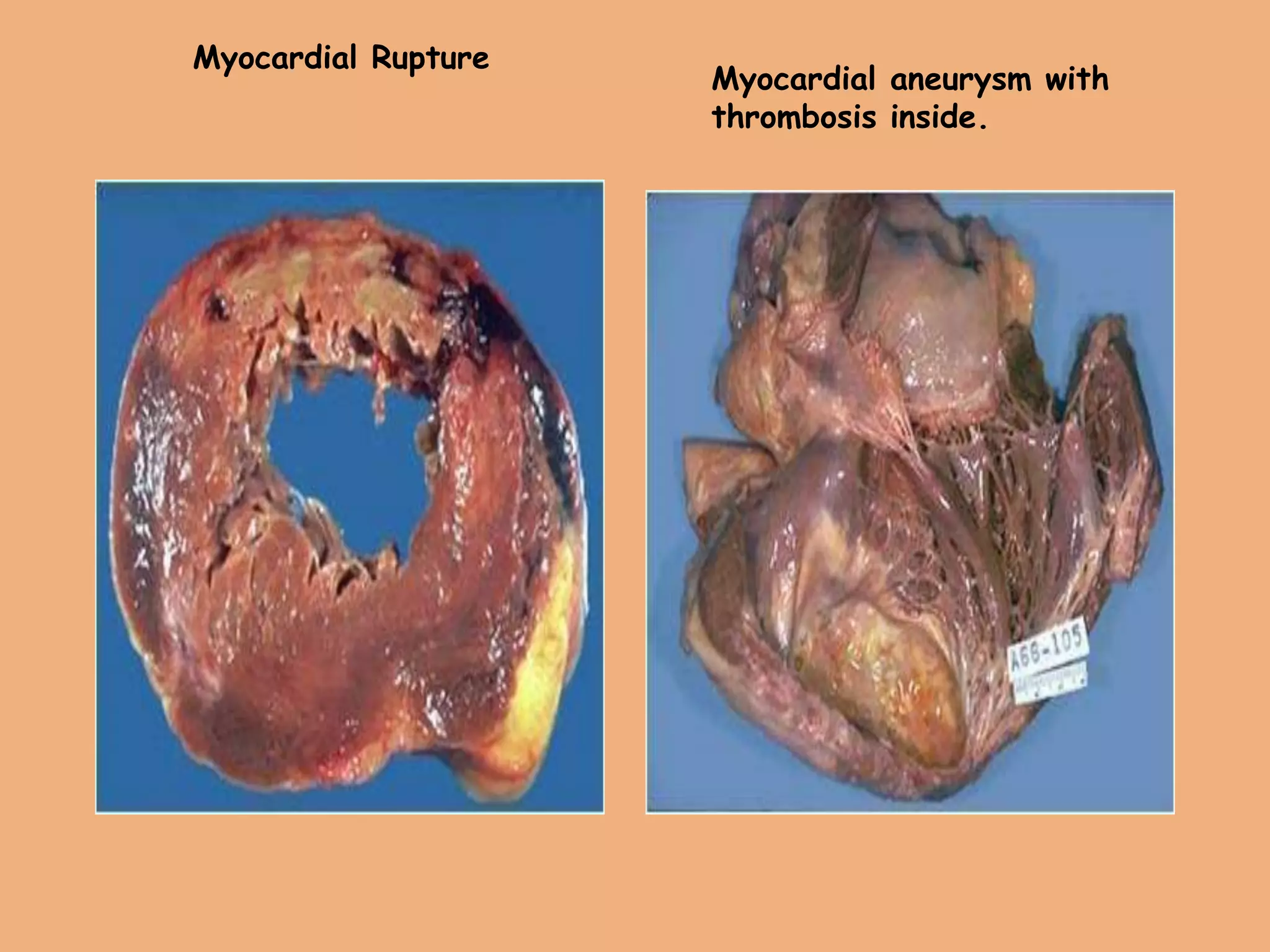
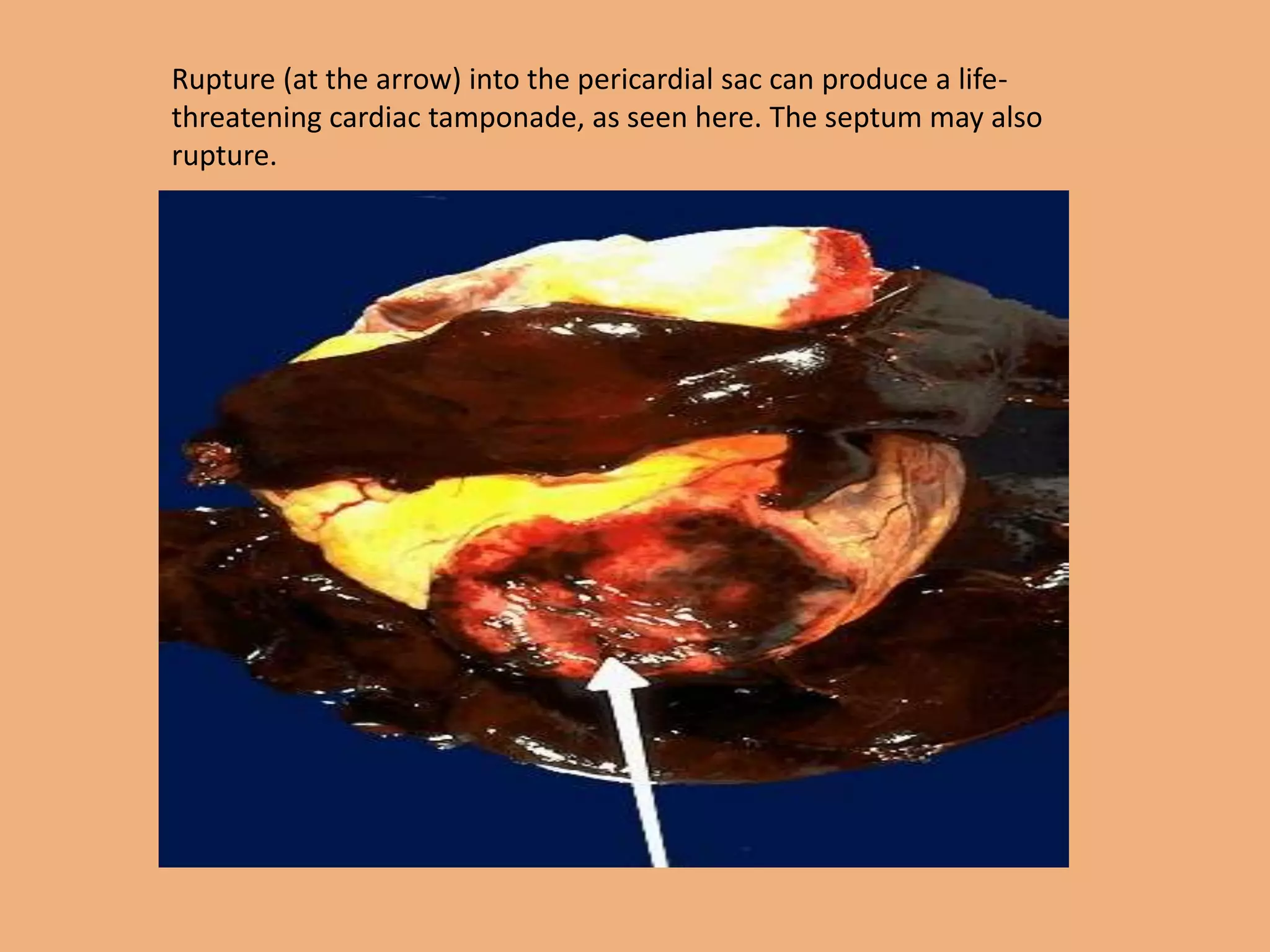
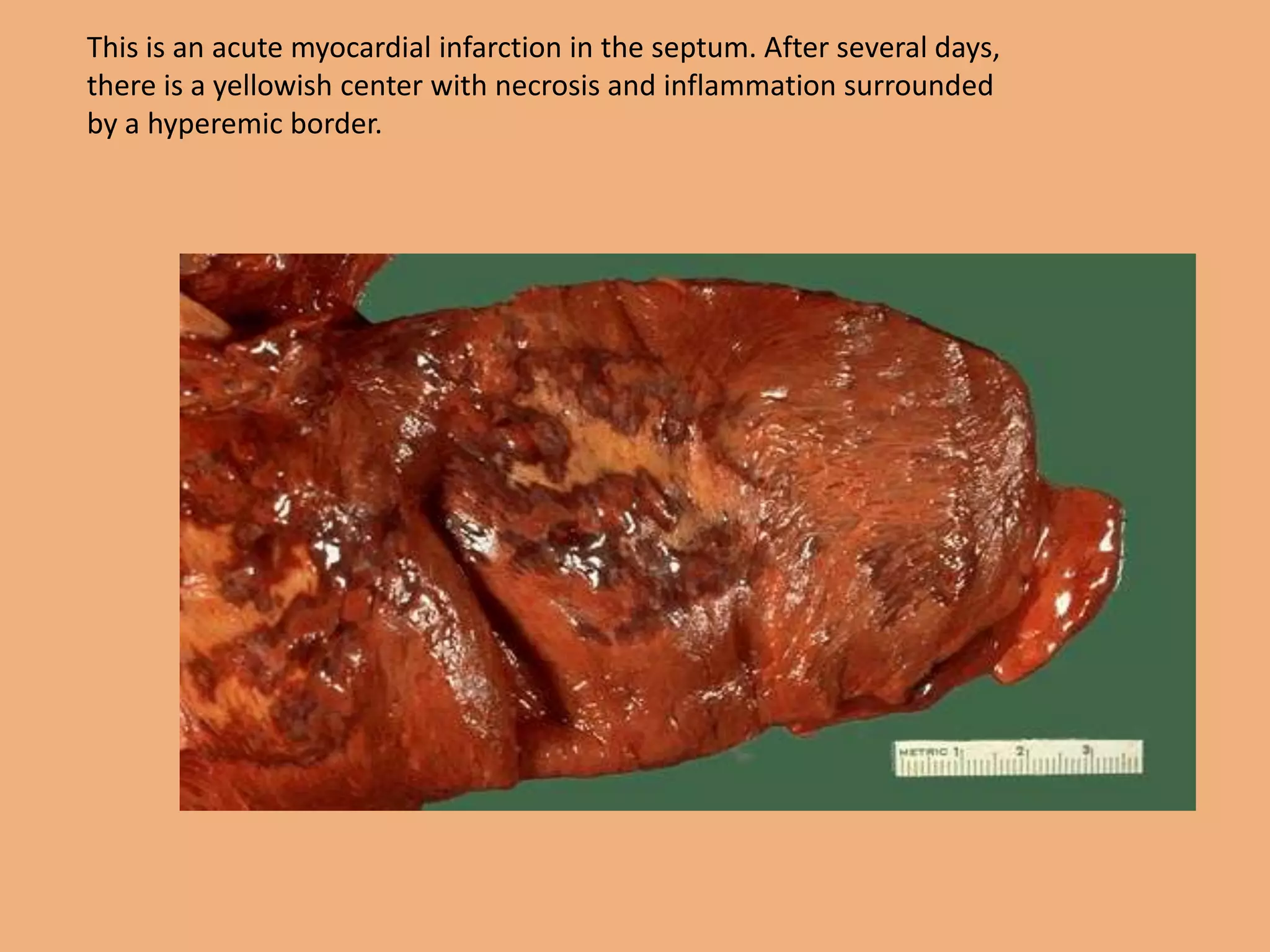
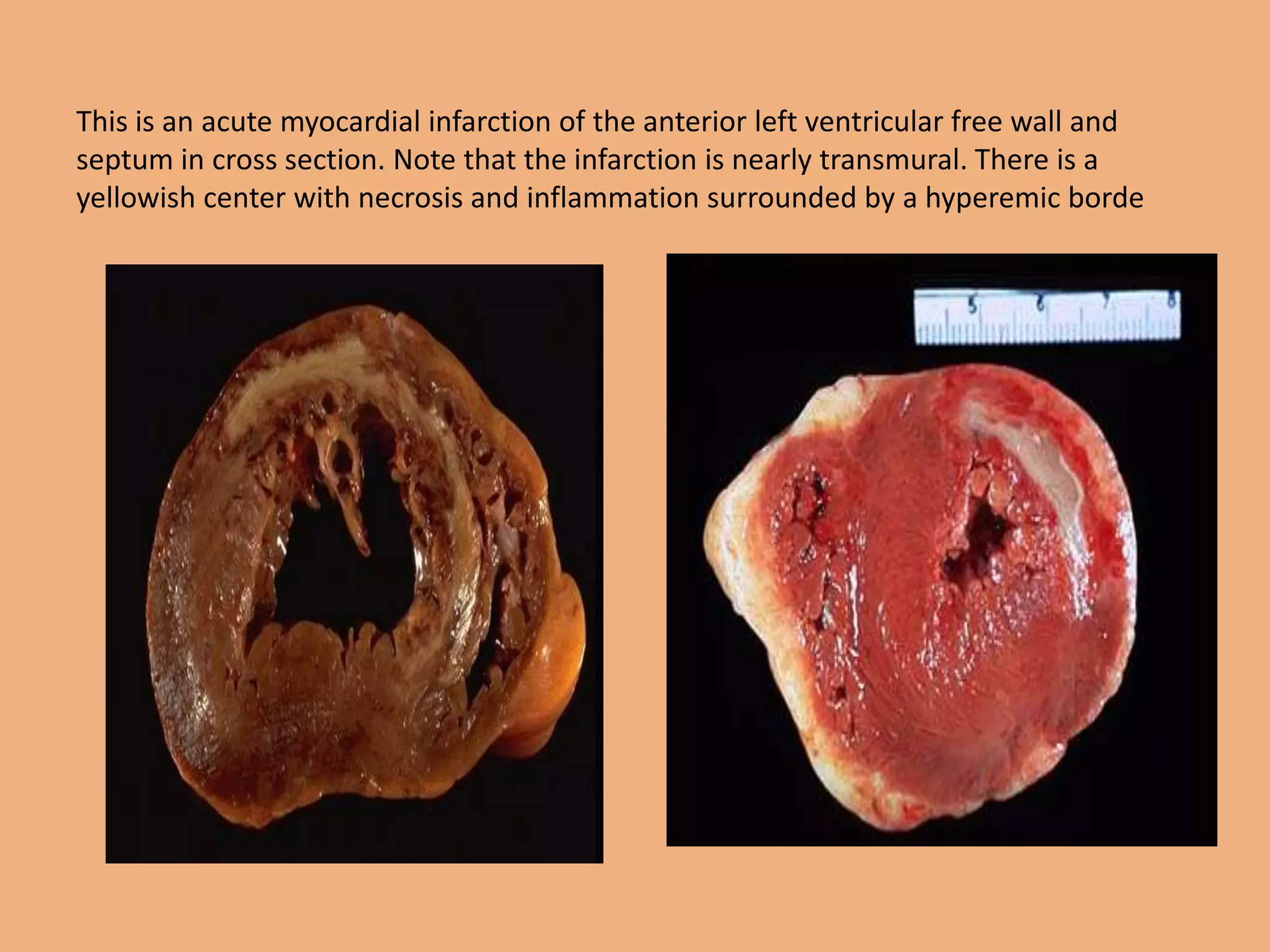
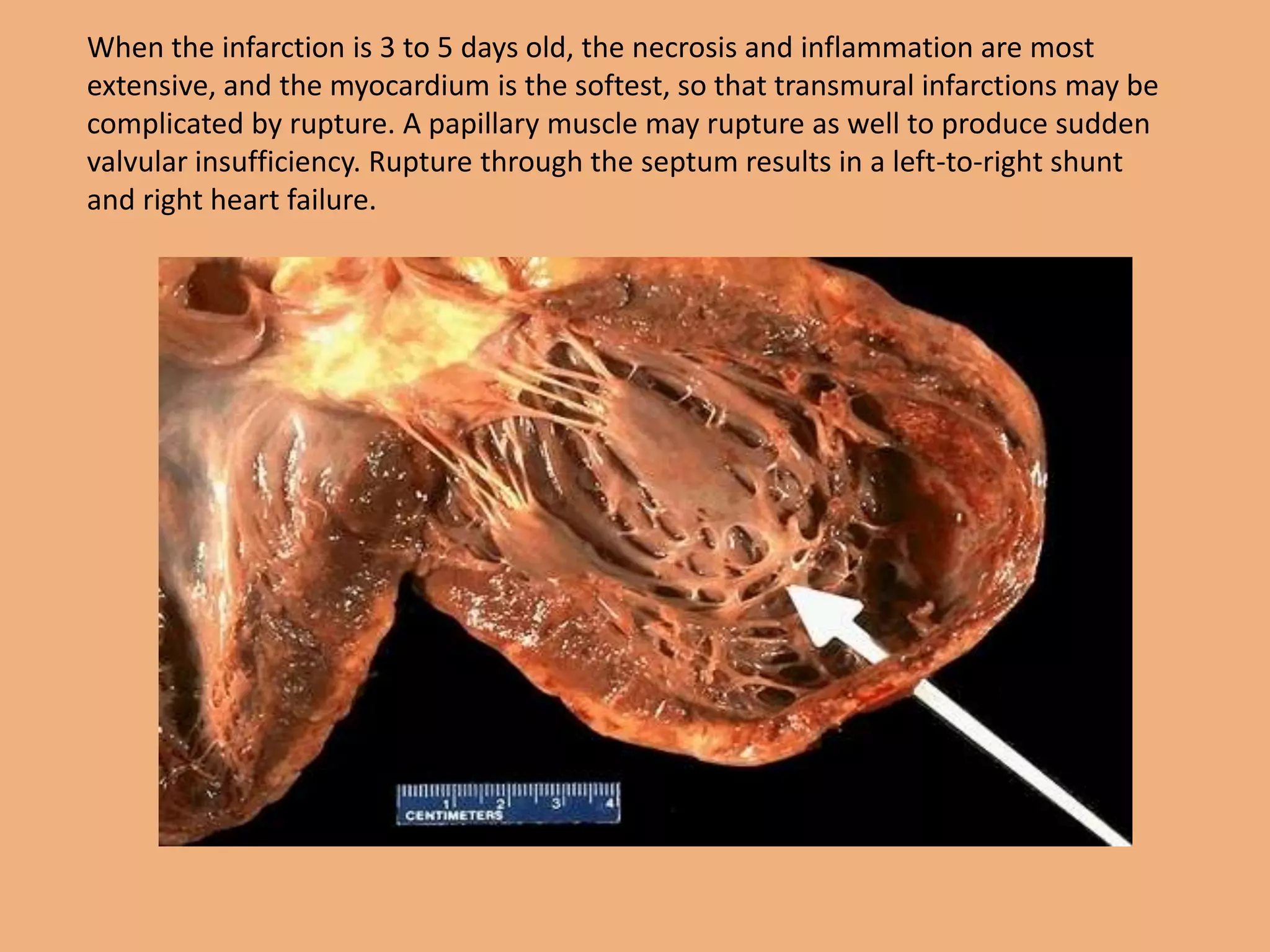
Myocardial infarction occurs when a coronary artery becomes blocked, interrupting blood flow to heart muscle. This causes damage and permanent loss of contraction in that portion of the heart. Over time, the affected area evolves from pallor to yellowing to fibrosis as dead heart cells are removed and replaced by scar tissue. Microscopically, early signs include wavy fibers at the border and loss of striations within infarcted regions. Complications can include arrhythmias, heart failure, mural thrombi, rupture and aneurysm formation depending on the size and location of the infarct. Examination of autopsy specimens involves analysis of coronary arteries and dissection of the heart to identify infarct location, extent and healing stage