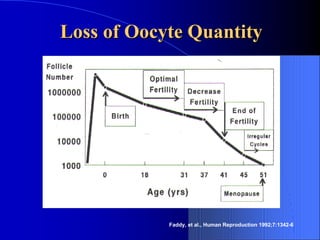
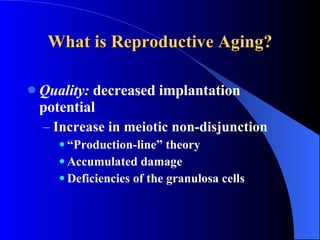
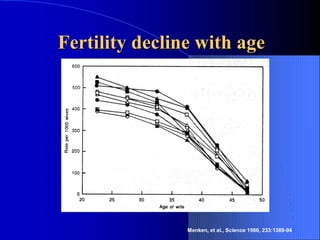
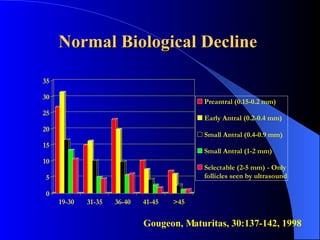
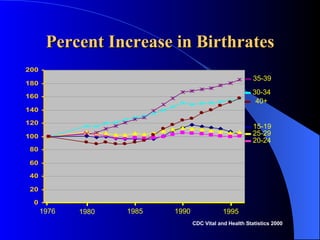
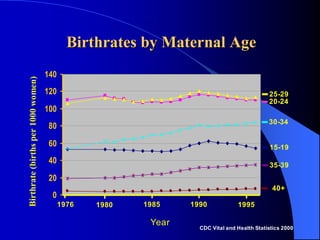
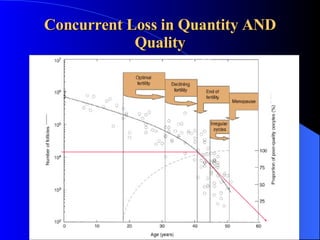
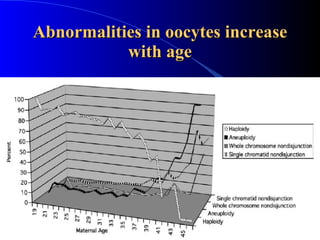
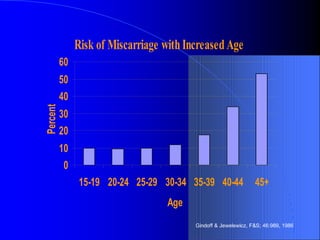
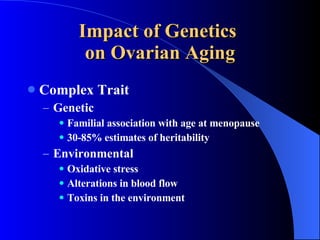
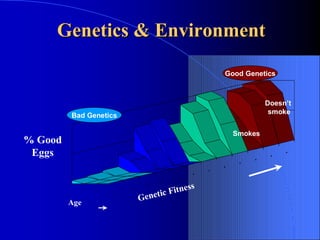
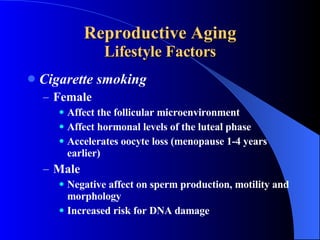
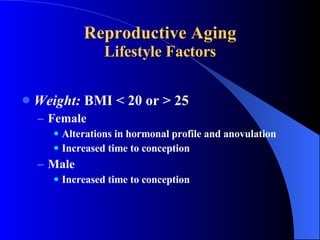
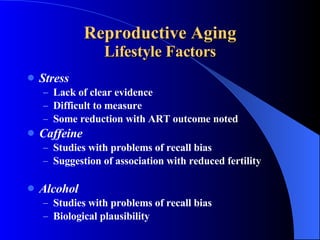
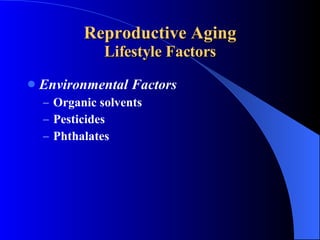
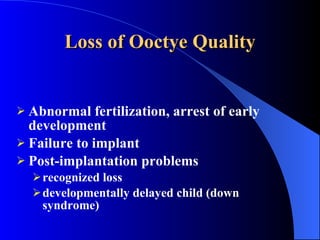
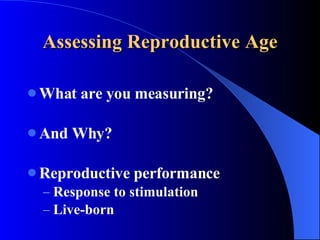
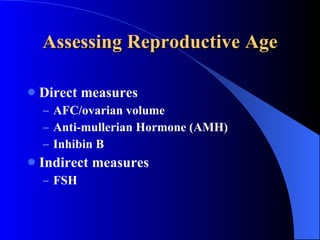
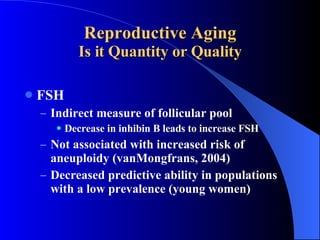
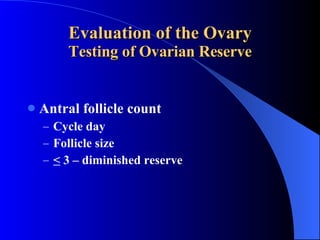
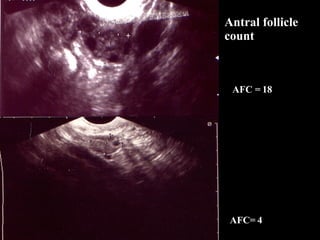
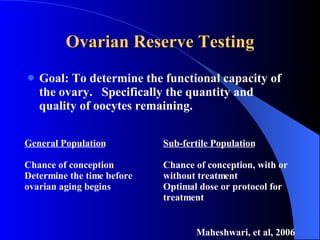
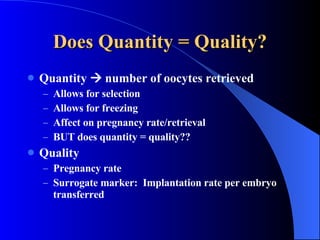
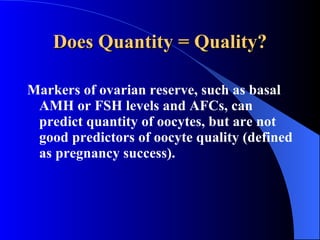
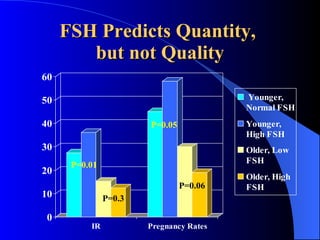
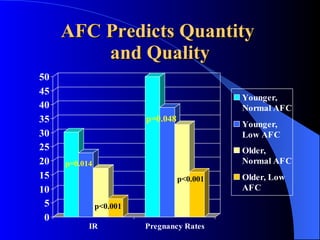
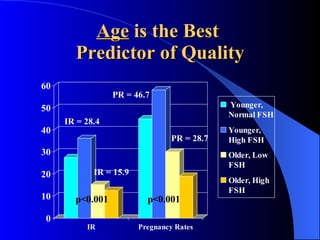
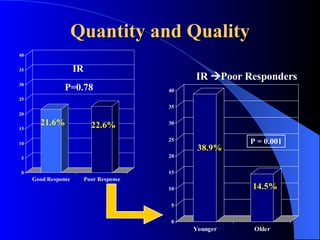
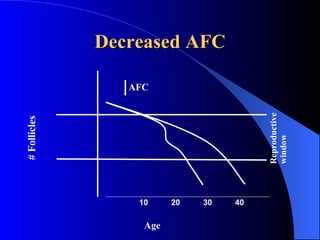
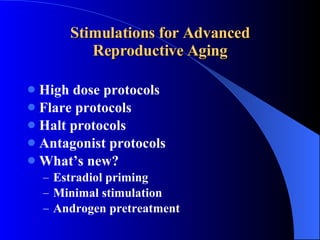
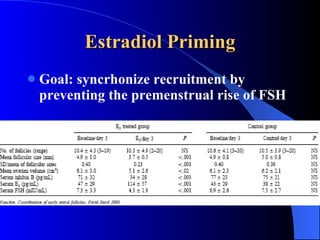
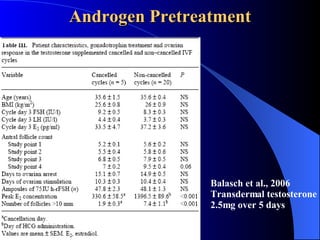
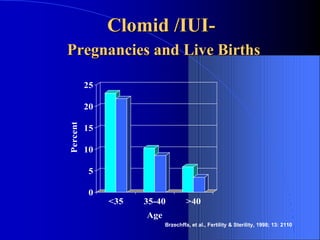
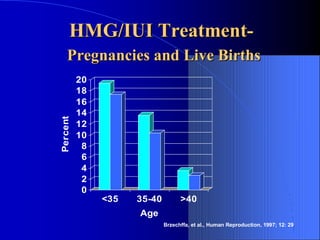
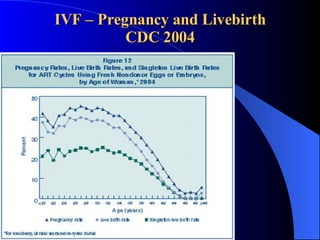
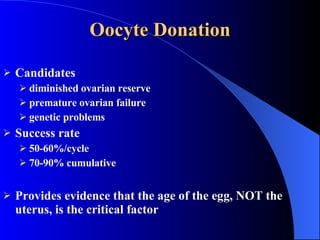
The document discusses reproductive aging and its impact on fertility. It notes that a woman's quantity and quality of eggs naturally declines with age starting in her mid-30s. While lifestyle factors like smoking can accelerate this decline, age remains the strongest predictor of egg quality and IVF success rates. The document reviews tests of ovarian reserve and treatments for advanced reproductive aging, concluding it's important to counsel patients on realistic expectations and consider alternatives like egg donation if natural conception is unlikely within 3-4 months.