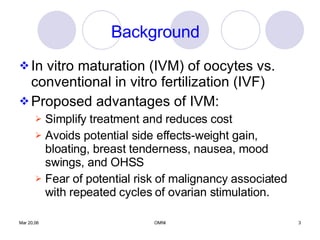
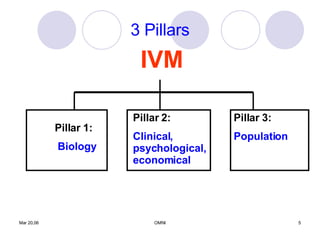
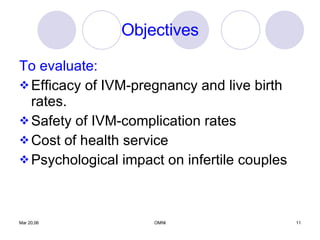
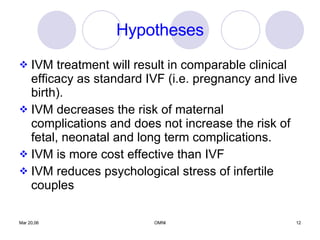
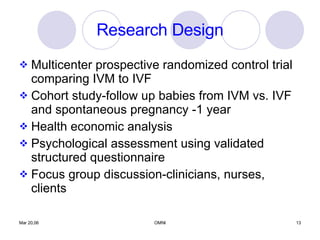
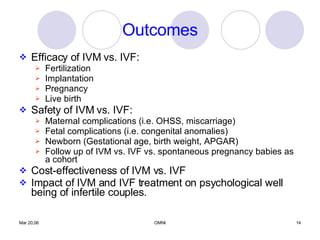
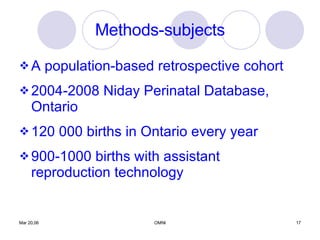
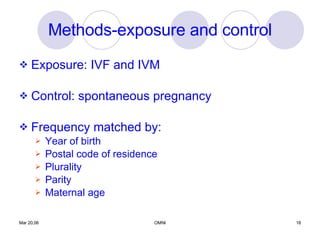
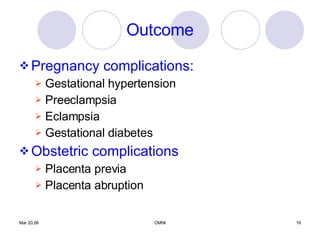
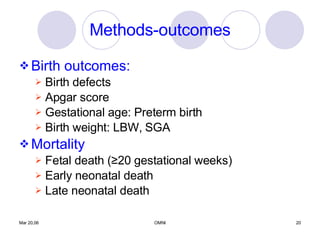
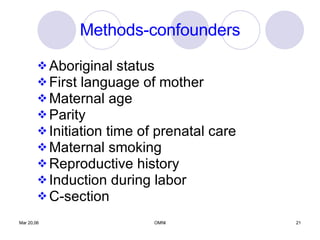
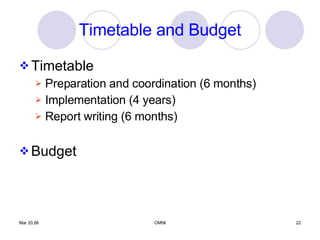
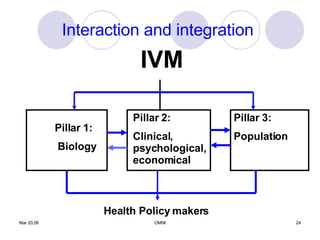
This document outlines a proposed transdisciplinary study to assess in vitro maturation (IVM) of oocytes as an alternative infertility treatment compared to conventional in vitro fertilization (IVF). The study would have three pillars: 1) comparing the biology of IVM and IVF through animal studies; 2) evaluating the clinical efficacy, safety, costs and psychological impacts of IVM versus IVF through human studies; and 3) studying pregnancy complications and birth outcomes from IVM, IVF and spontaneous pregnancies using population health data. The goal is to provide a comprehensive evaluation of IVM across biological, clinical, economic and population levels to determine its potential as a treatment option for infertile couples.