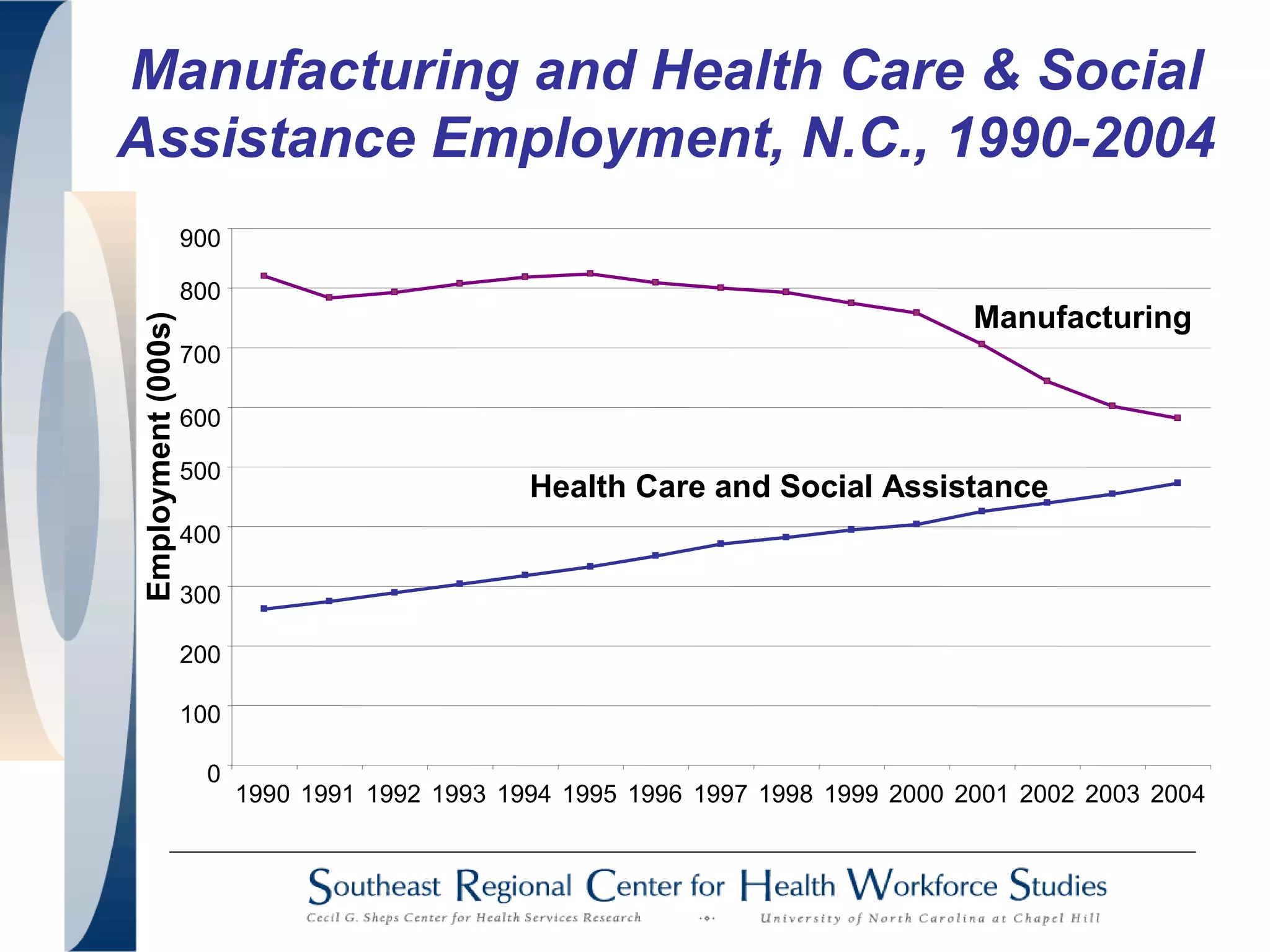
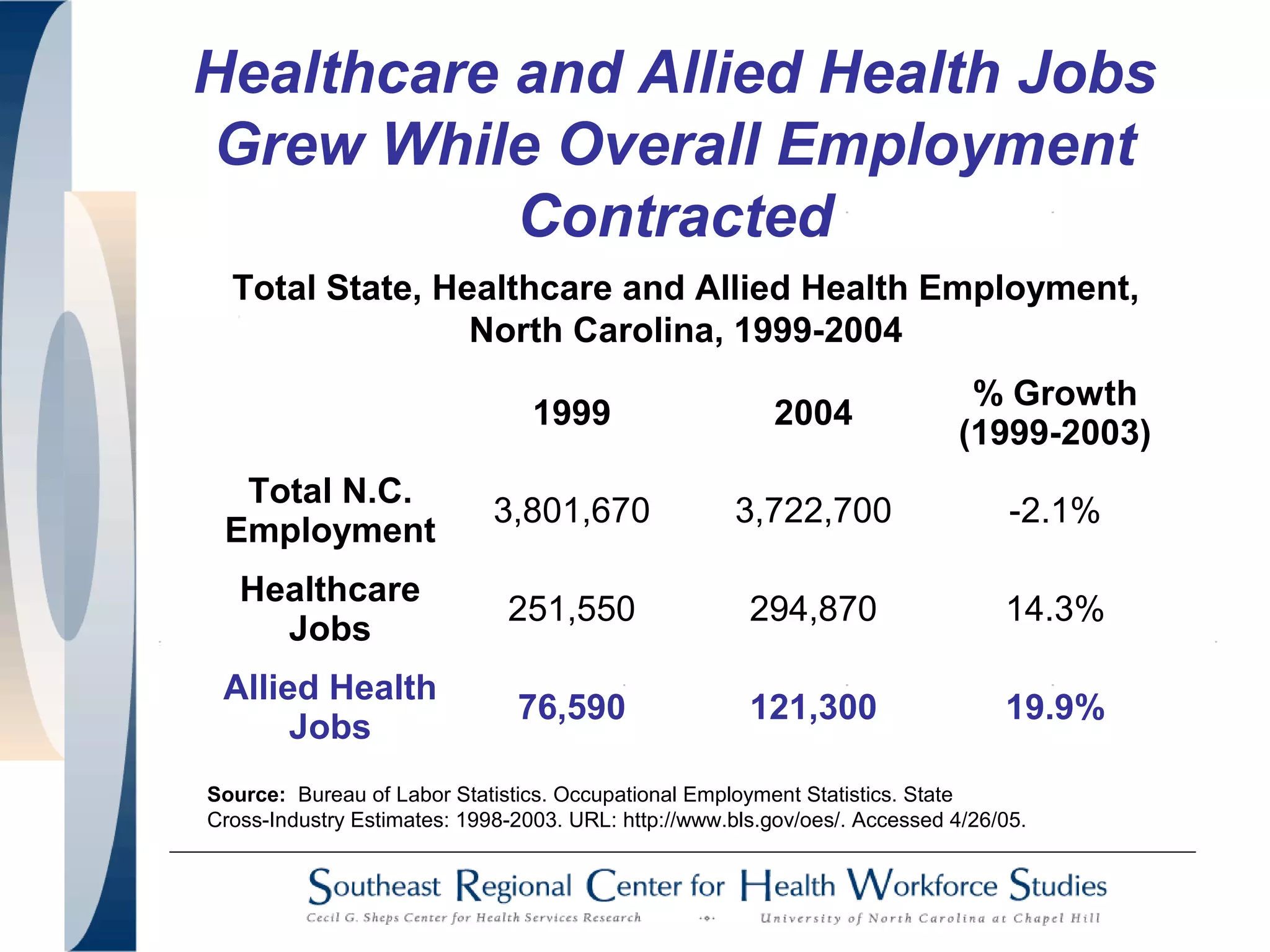
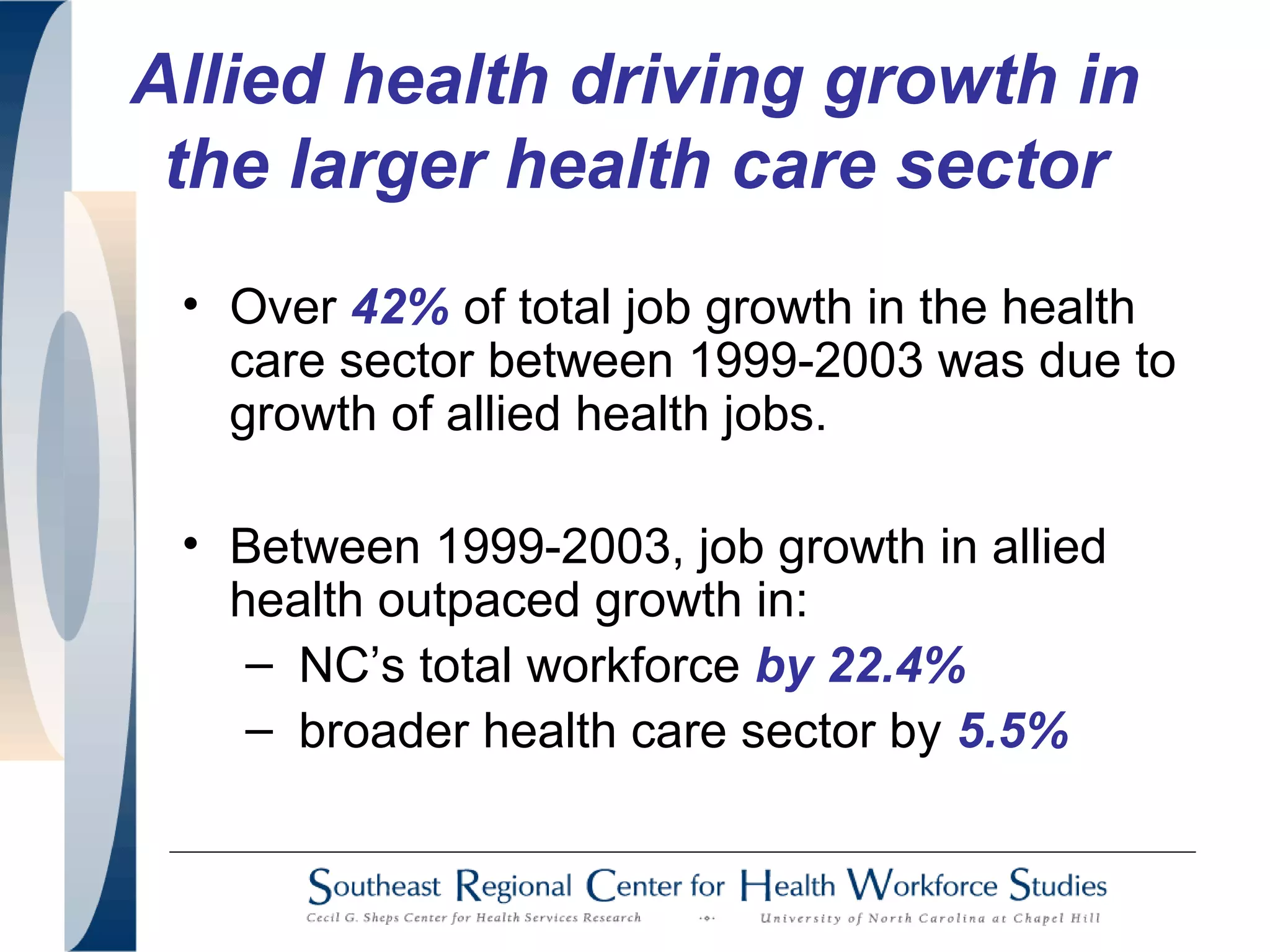
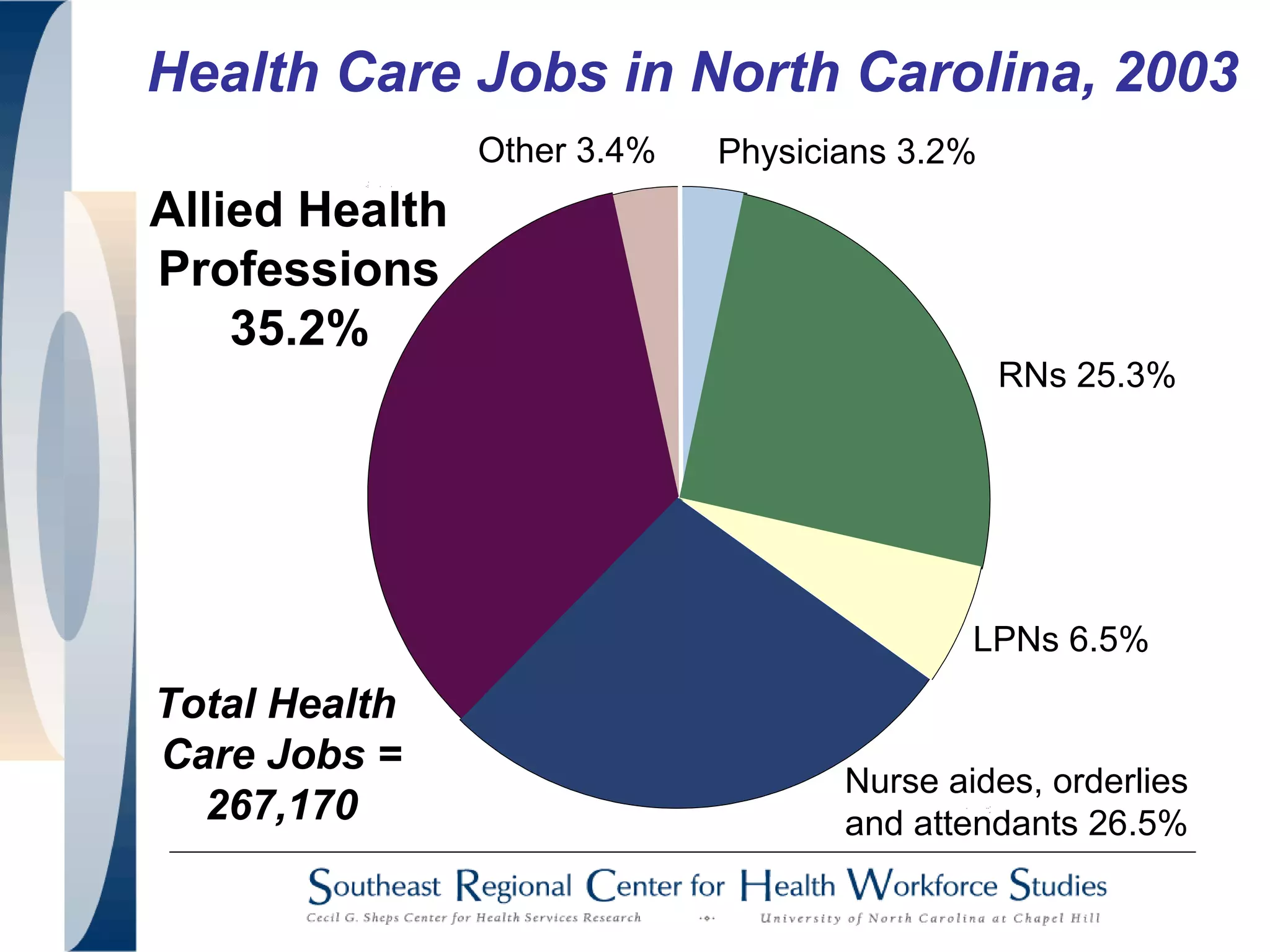
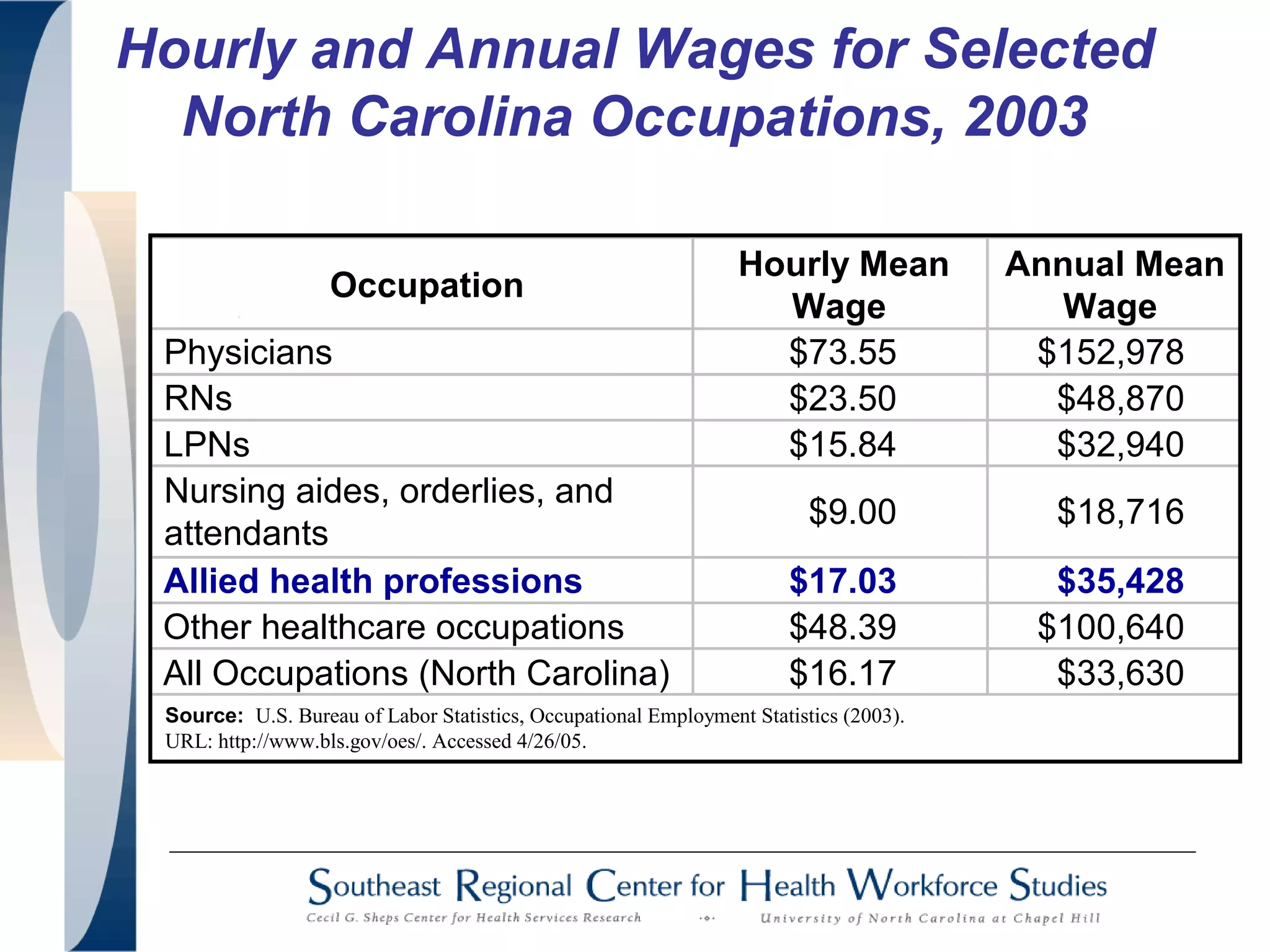
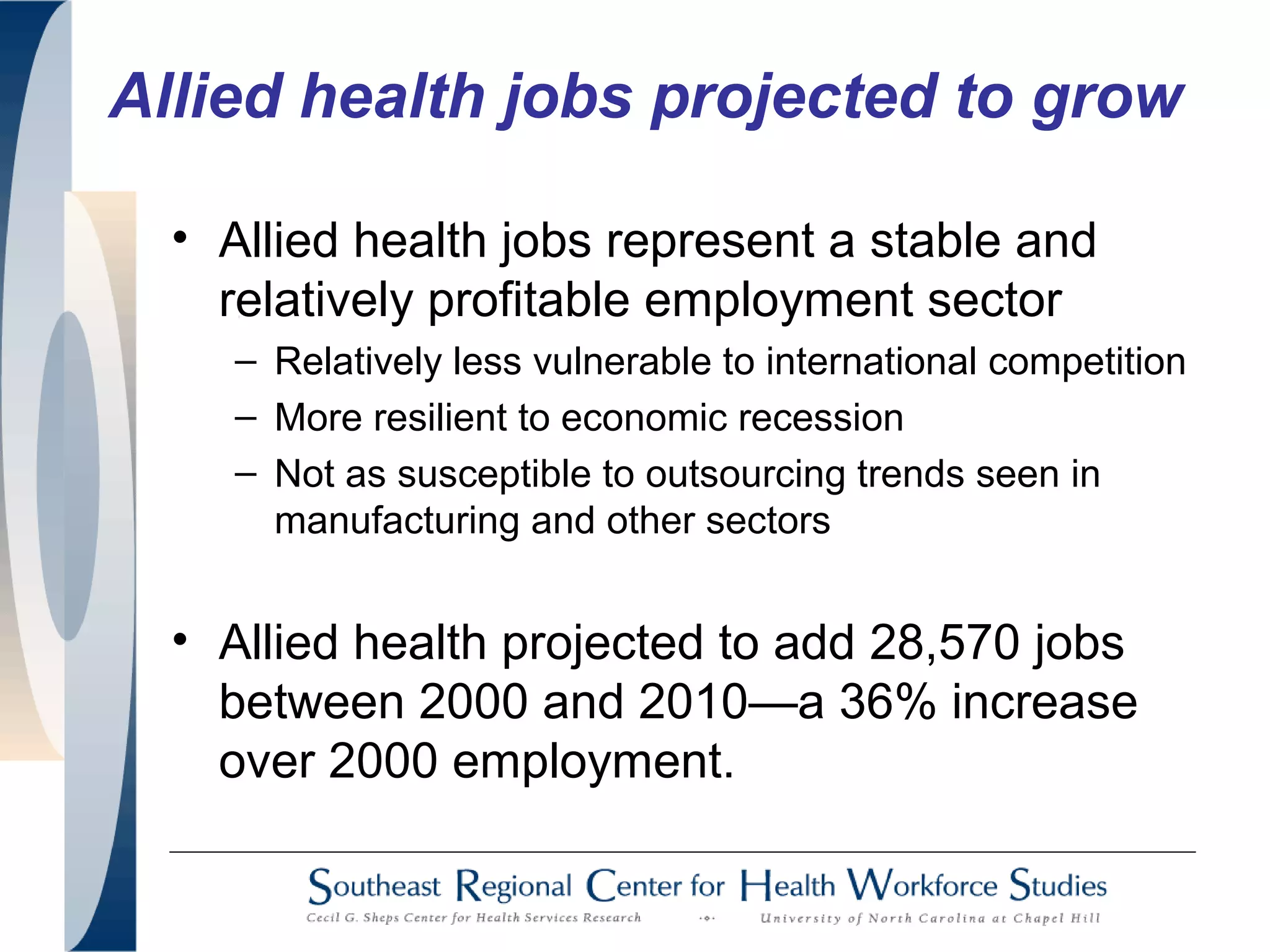
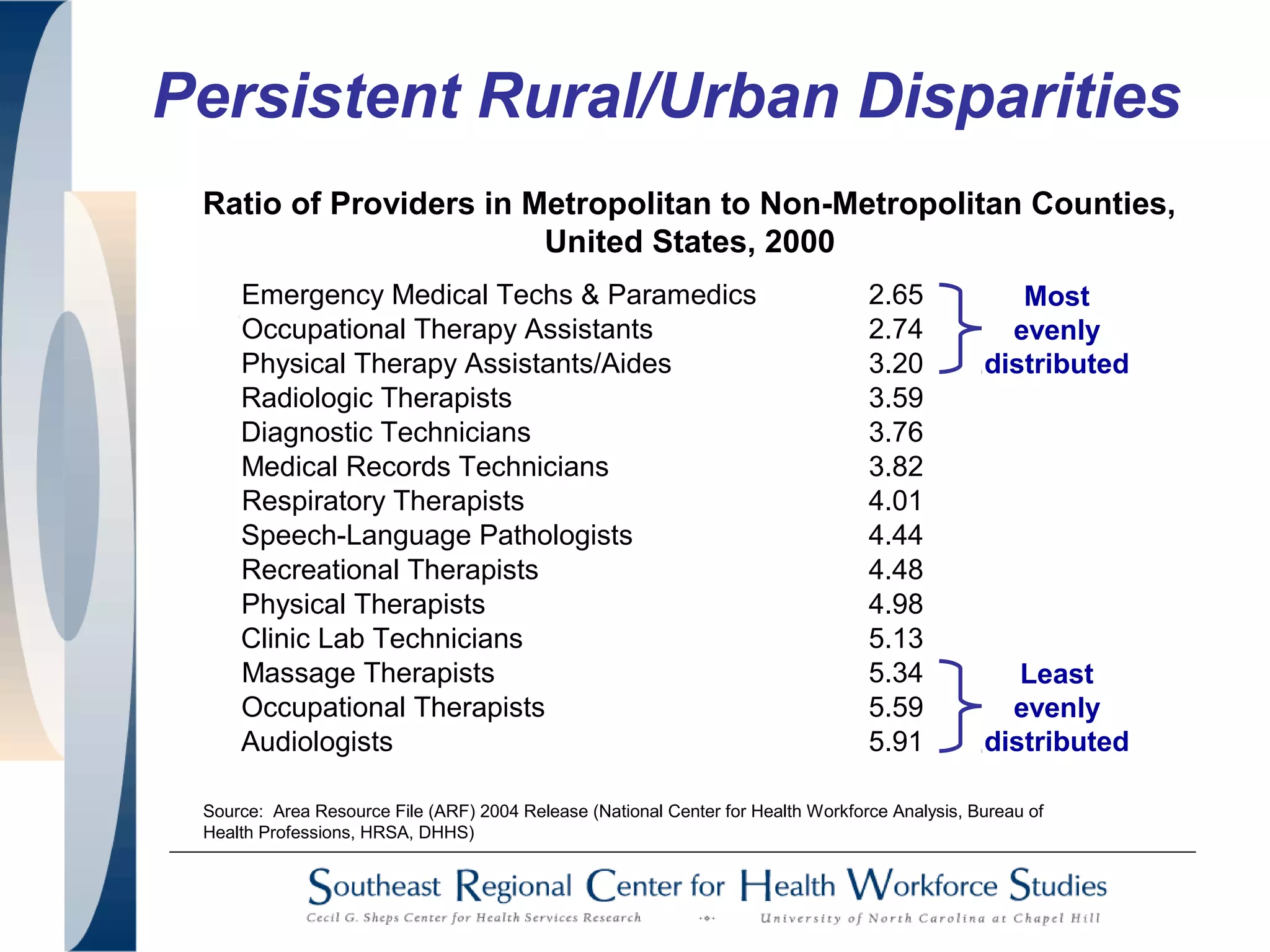
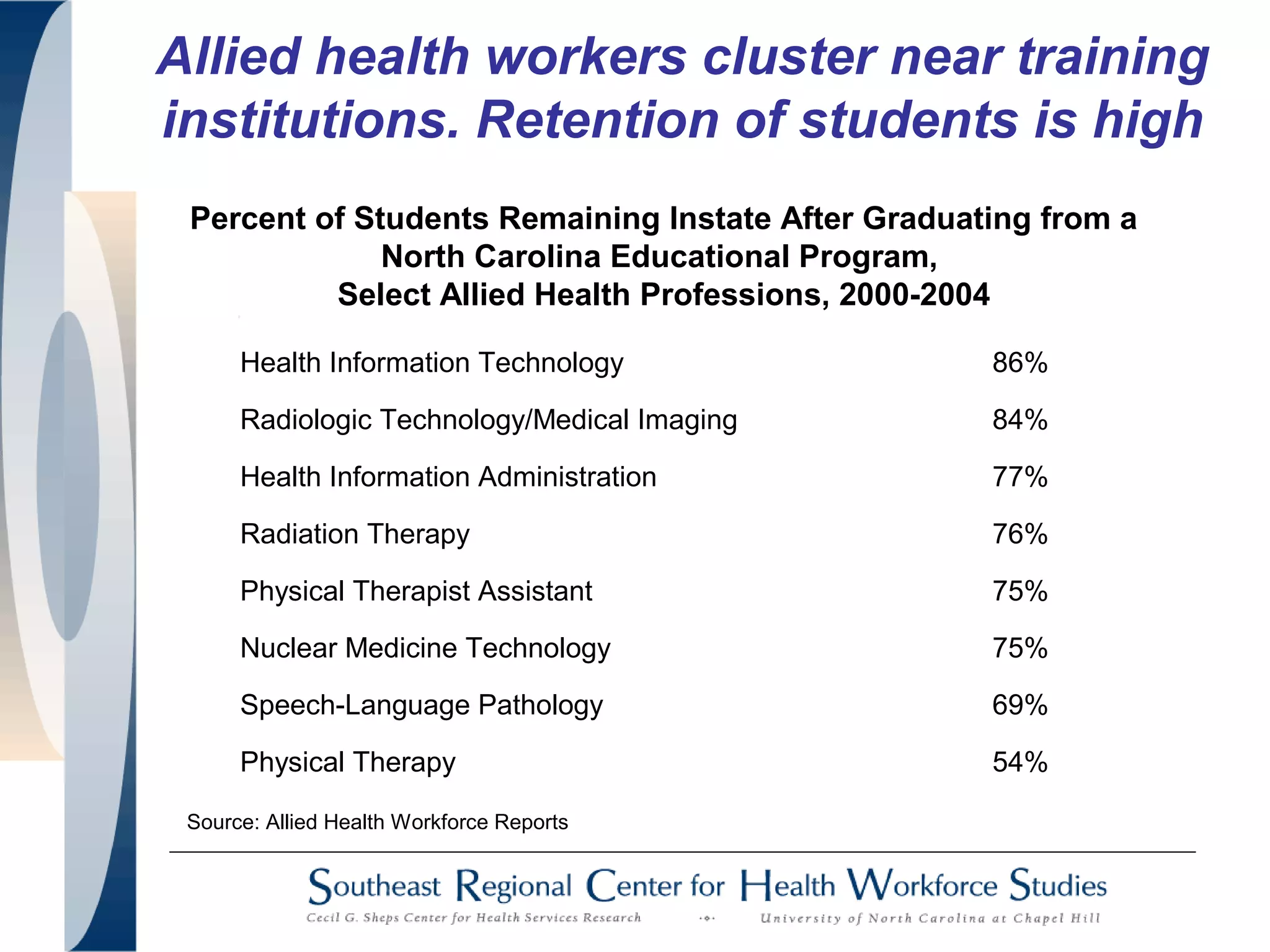
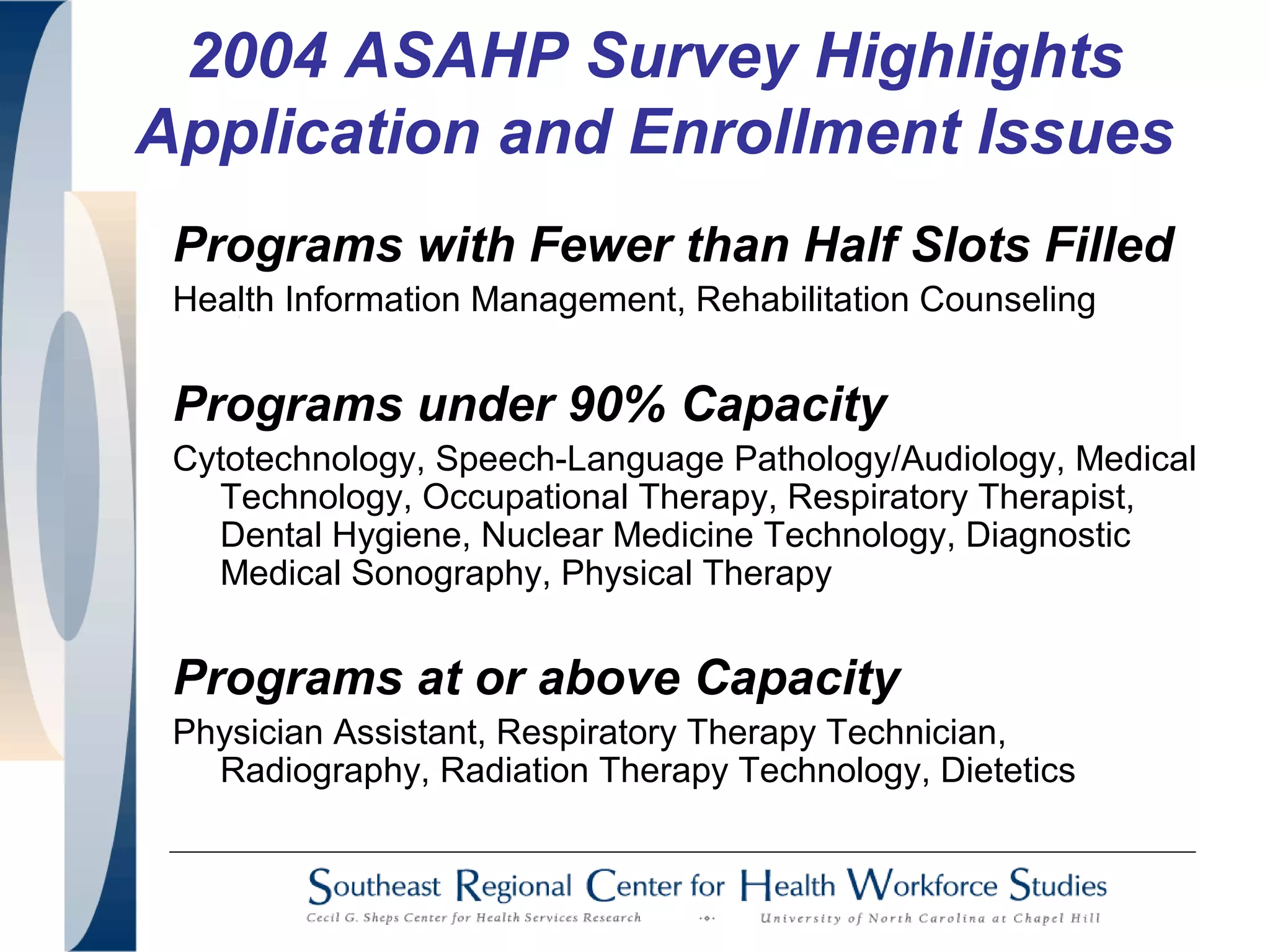
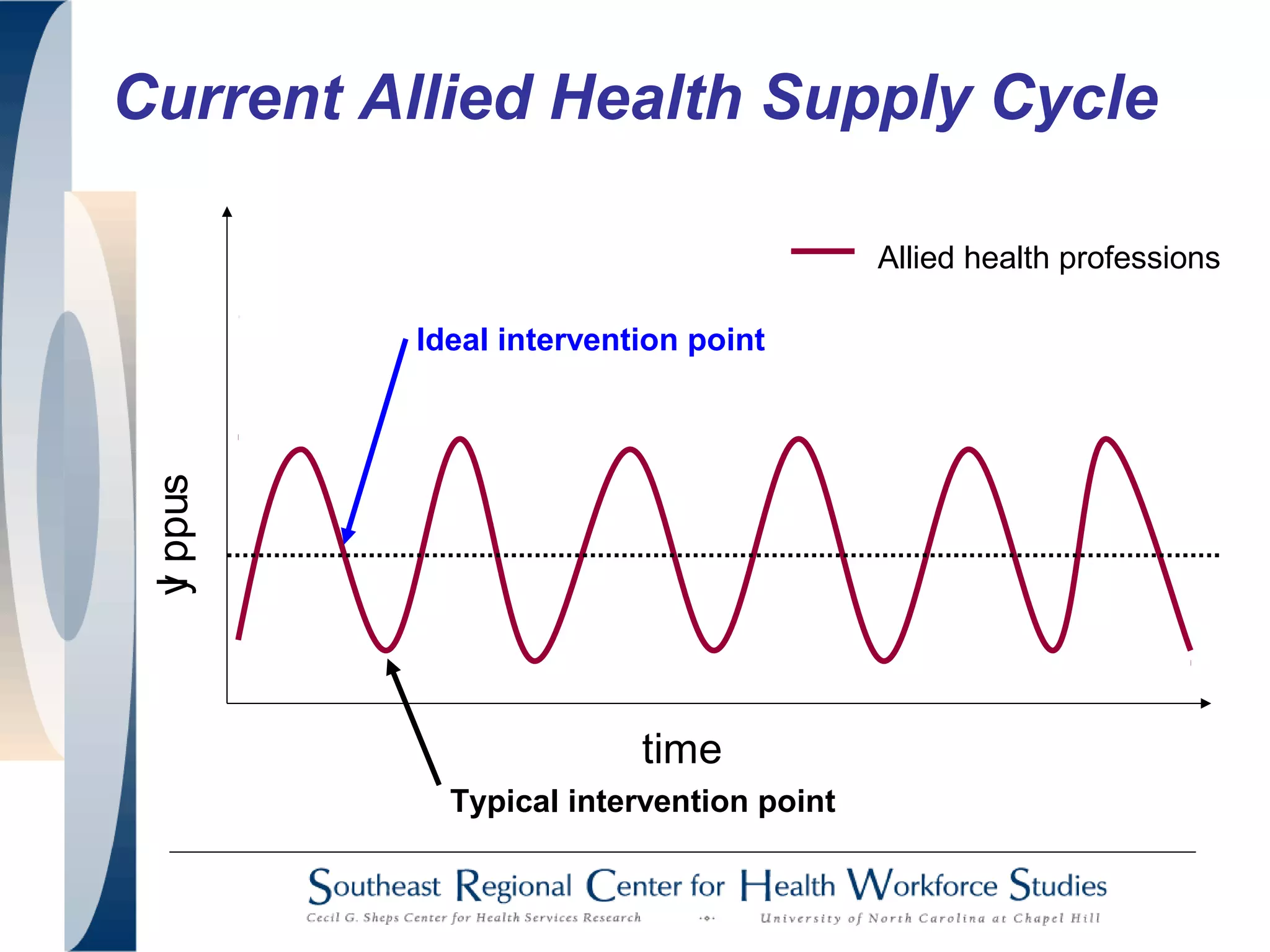
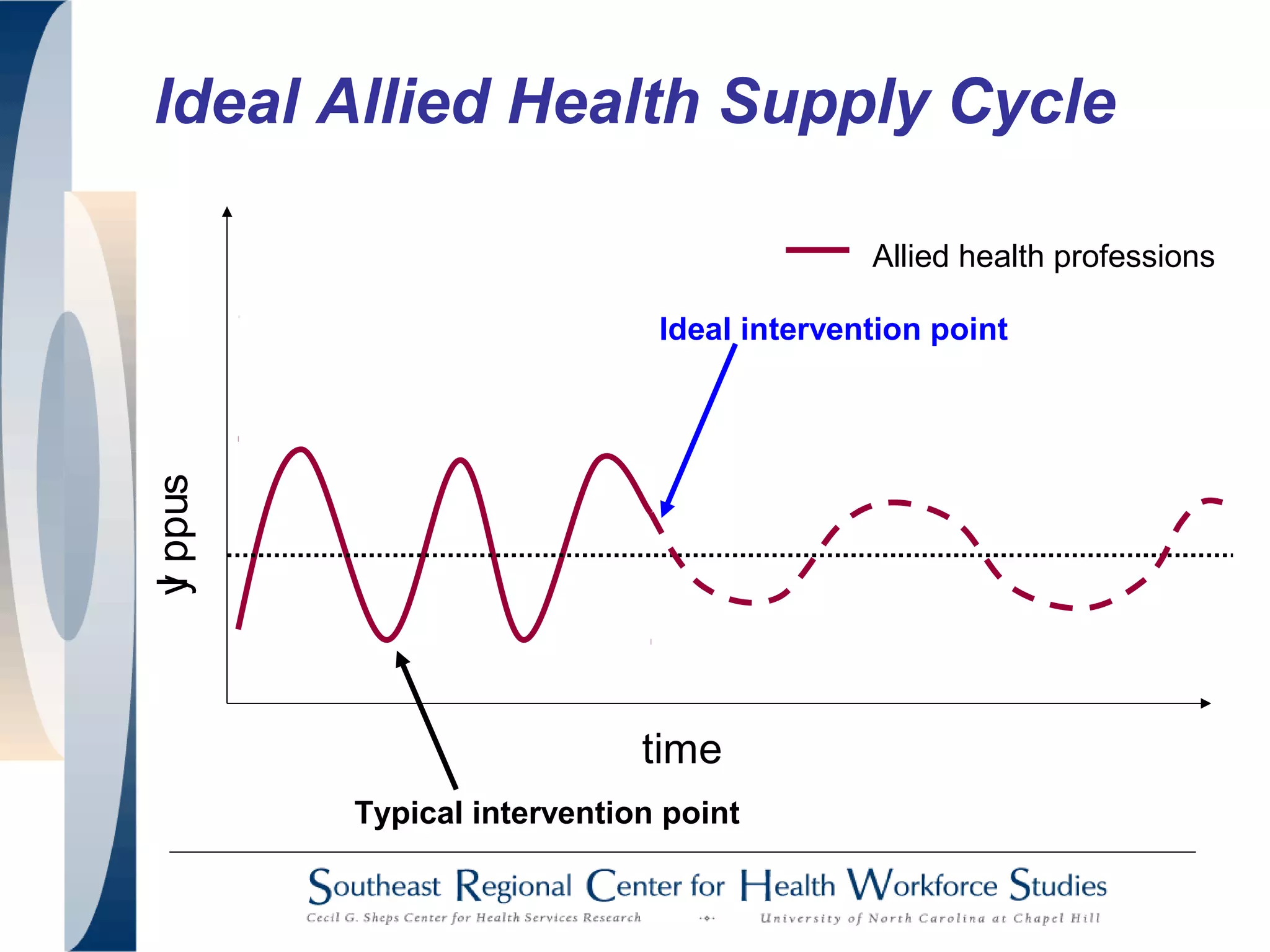
The document provides an overview of issues and opportunities facing the allied health workforce according to a 2005 report. It summarizes that allied health jobs are an important part of the healthcare sector and economy, growing while other sectors contracted. However, the report finds workforce challenges including disparities between urban and rural areas, attrition in educational programs, faculty shortages, and lack of clinical placements. It recommends improving data collection, framing data in an economic context, and developing better workforce planning infrastructure to address shortages and ensure access to trained allied health professionals.