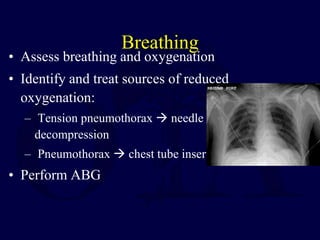
Polytrauma is a leading cause of death and disability in people under 45 years old. Mortality after trauma can be immediate from severe injuries like brain injuries or blood vessel transections, or delayed from complications like sepsis or multiple organ failure. Trauma centers and damage control tactics can reduce early and delayed mortality. Advanced Trauma Life Support (ATLS) principles dictate treating the greatest threat to life first by performing a primary survey to assess the airway, breathing, circulation, disability, and exposure, with resuscitation occurring simultaneously. Injuries are then addressed in order of severity, with controlling hemorrhage being the top priority.