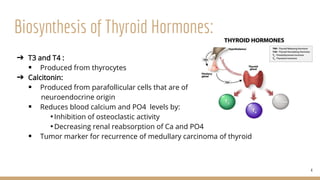
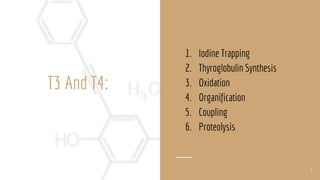
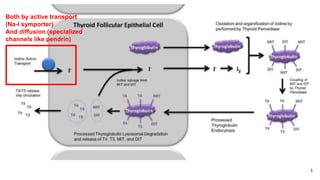
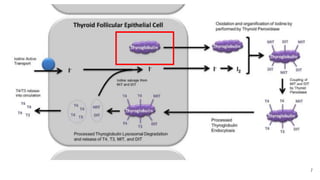
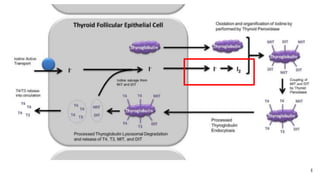
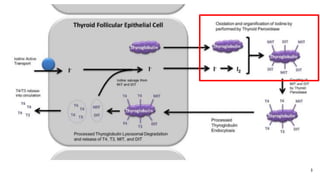
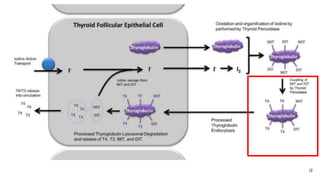
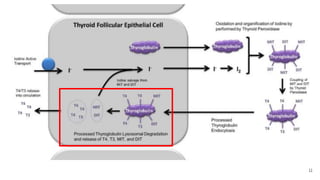
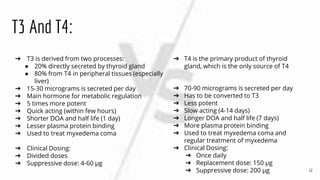
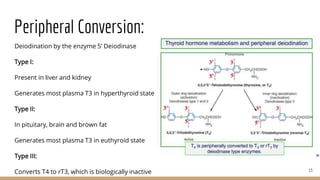
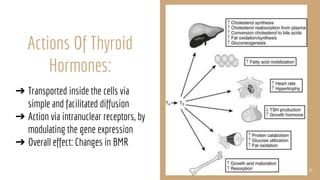
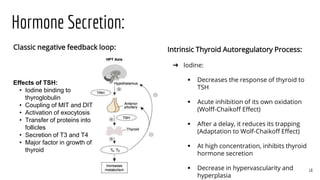
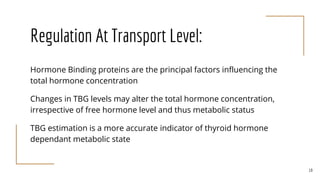
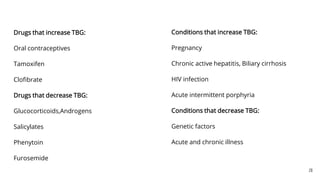
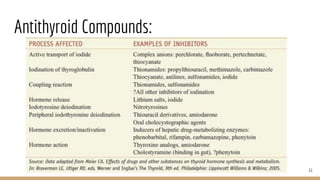
The document discusses the physiology of the thyroid gland, its role in metabolism regulation, and the biosynthesis of thyroid hormones T3 and T4. It details the processes involved in hormone production, regulation, actions, and the influence of various factors on hormone levels. It also covers transport mechanisms and the effects of TSH on thyroid function, alongside the impact of drugs and conditions on thyroid hormone concentrations.