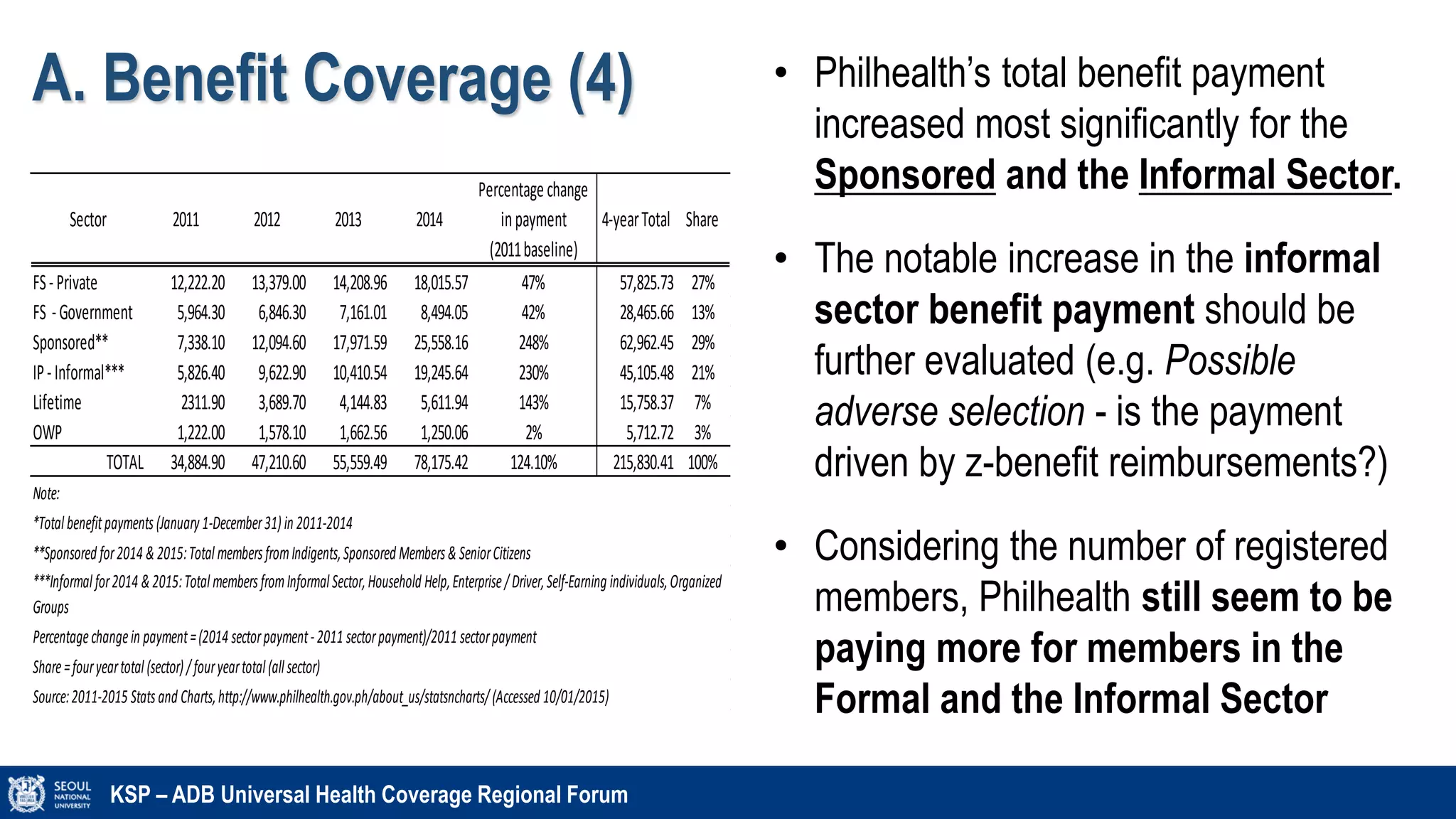
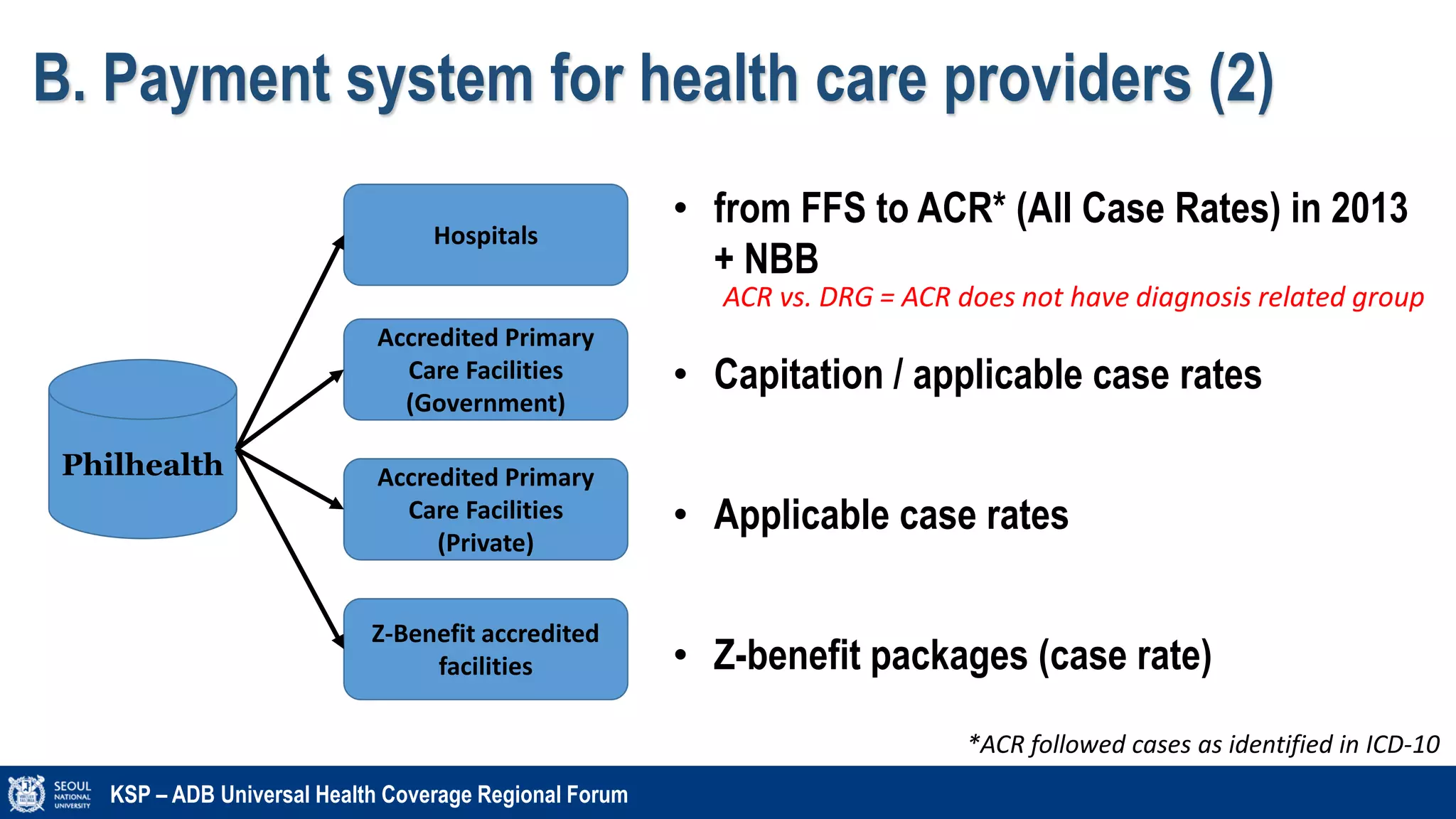
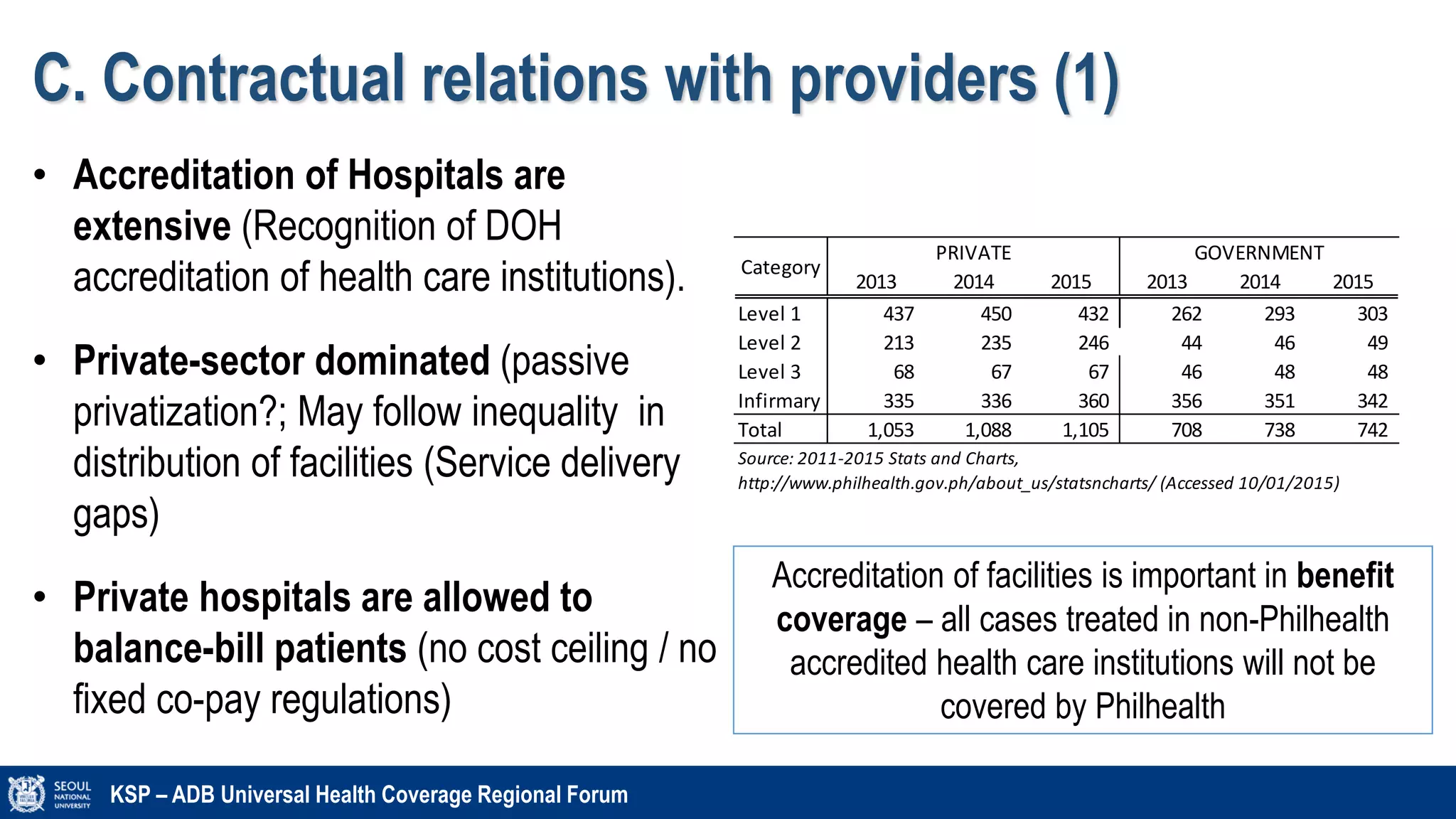
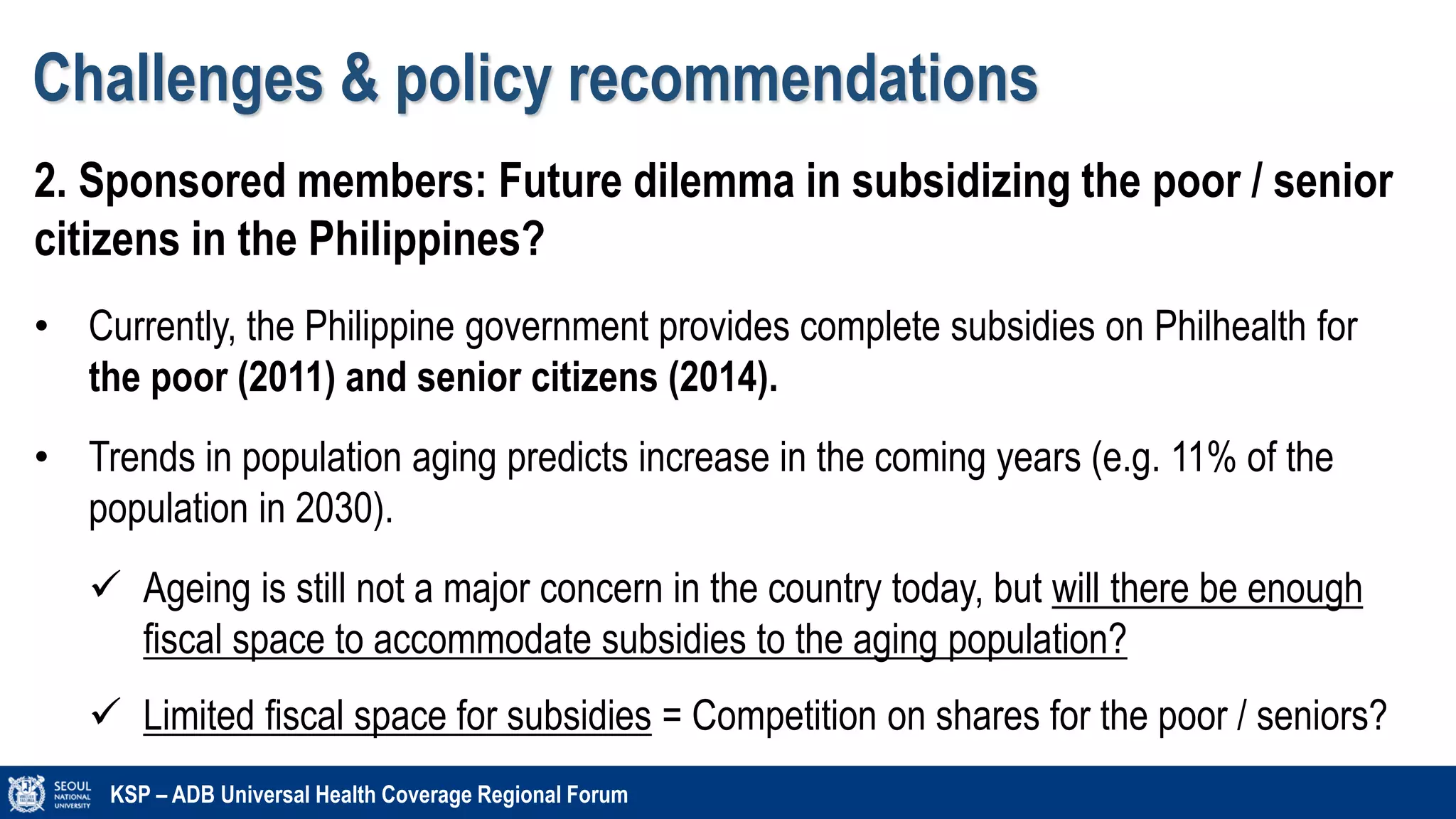
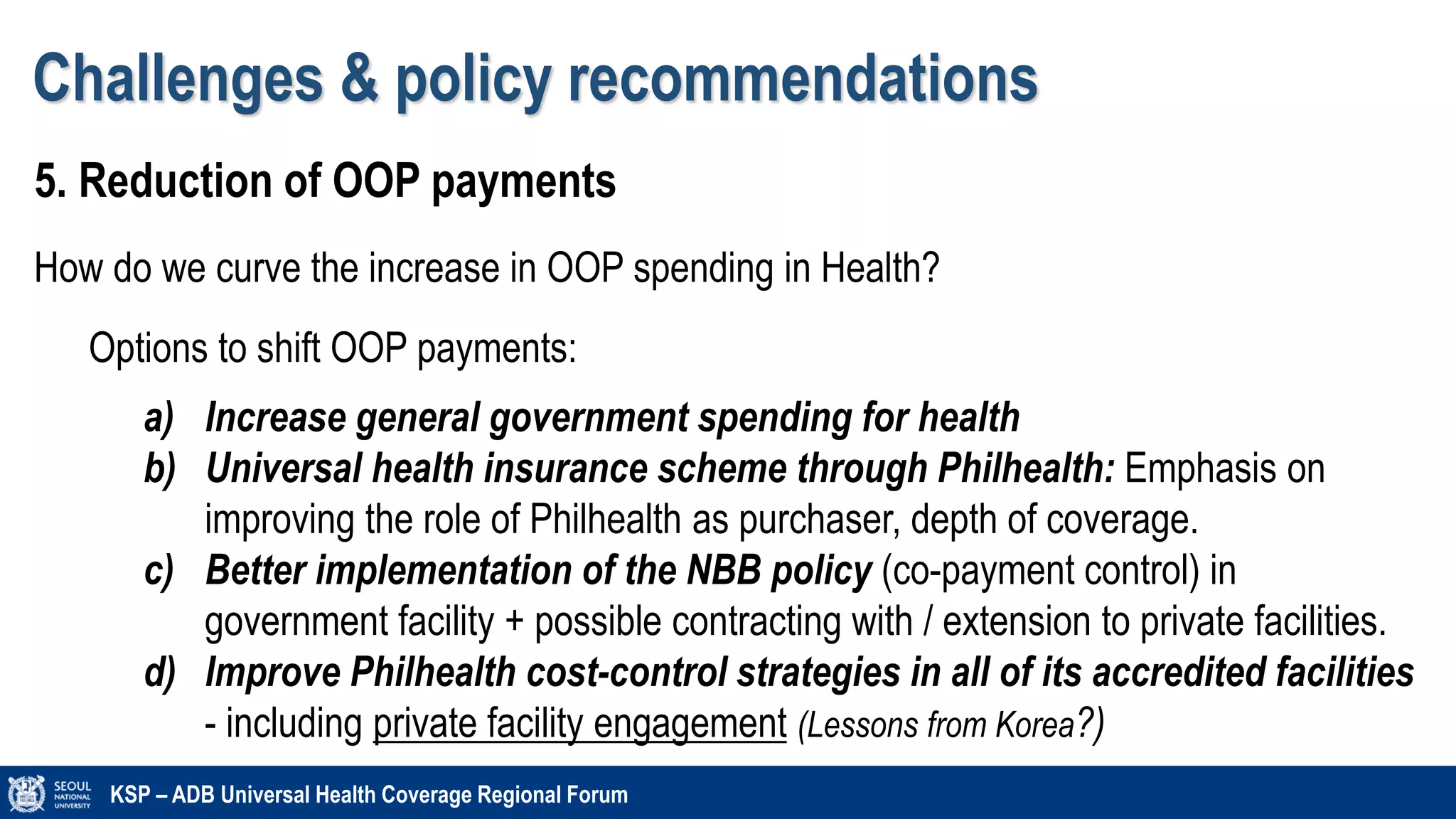
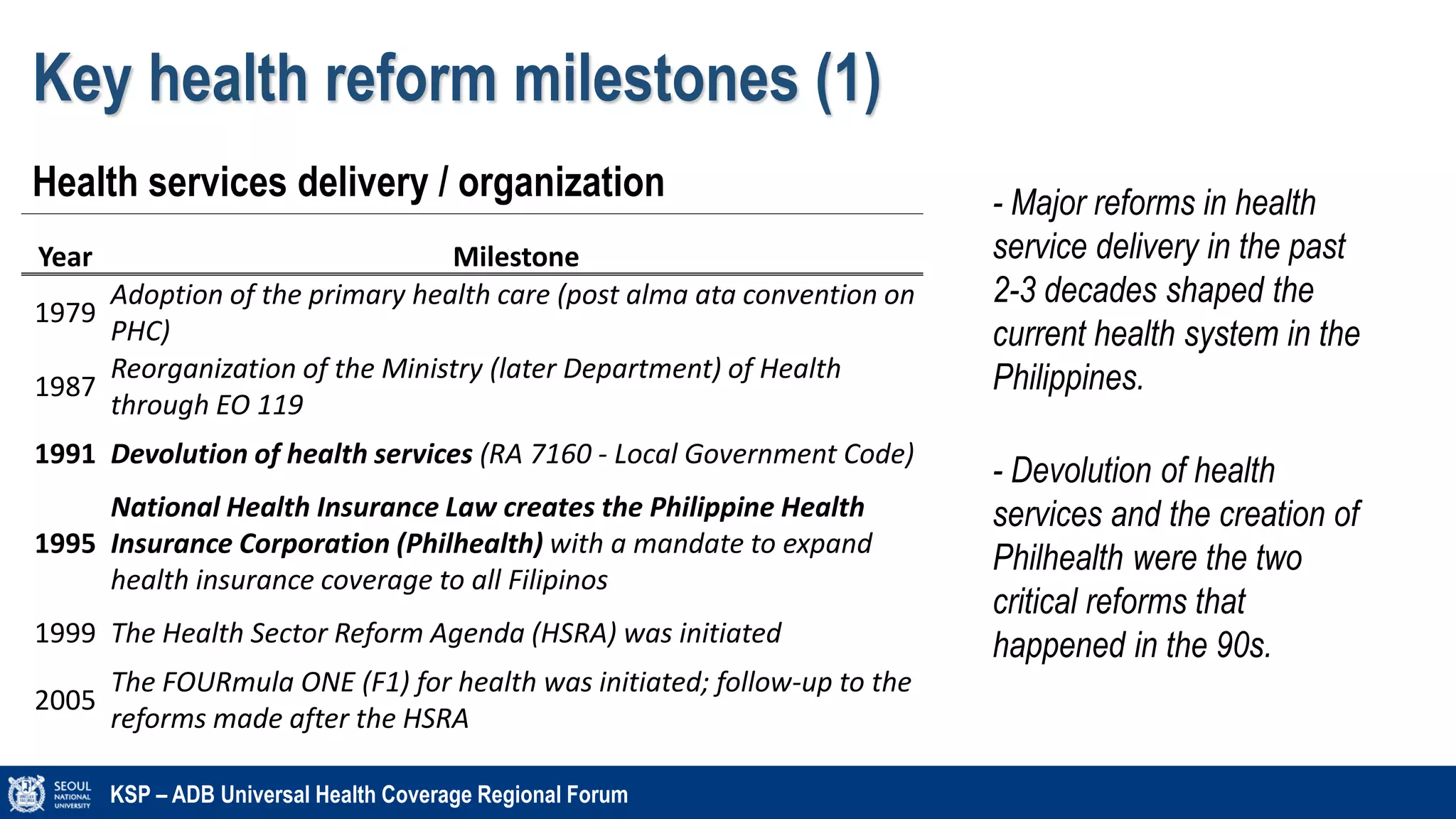
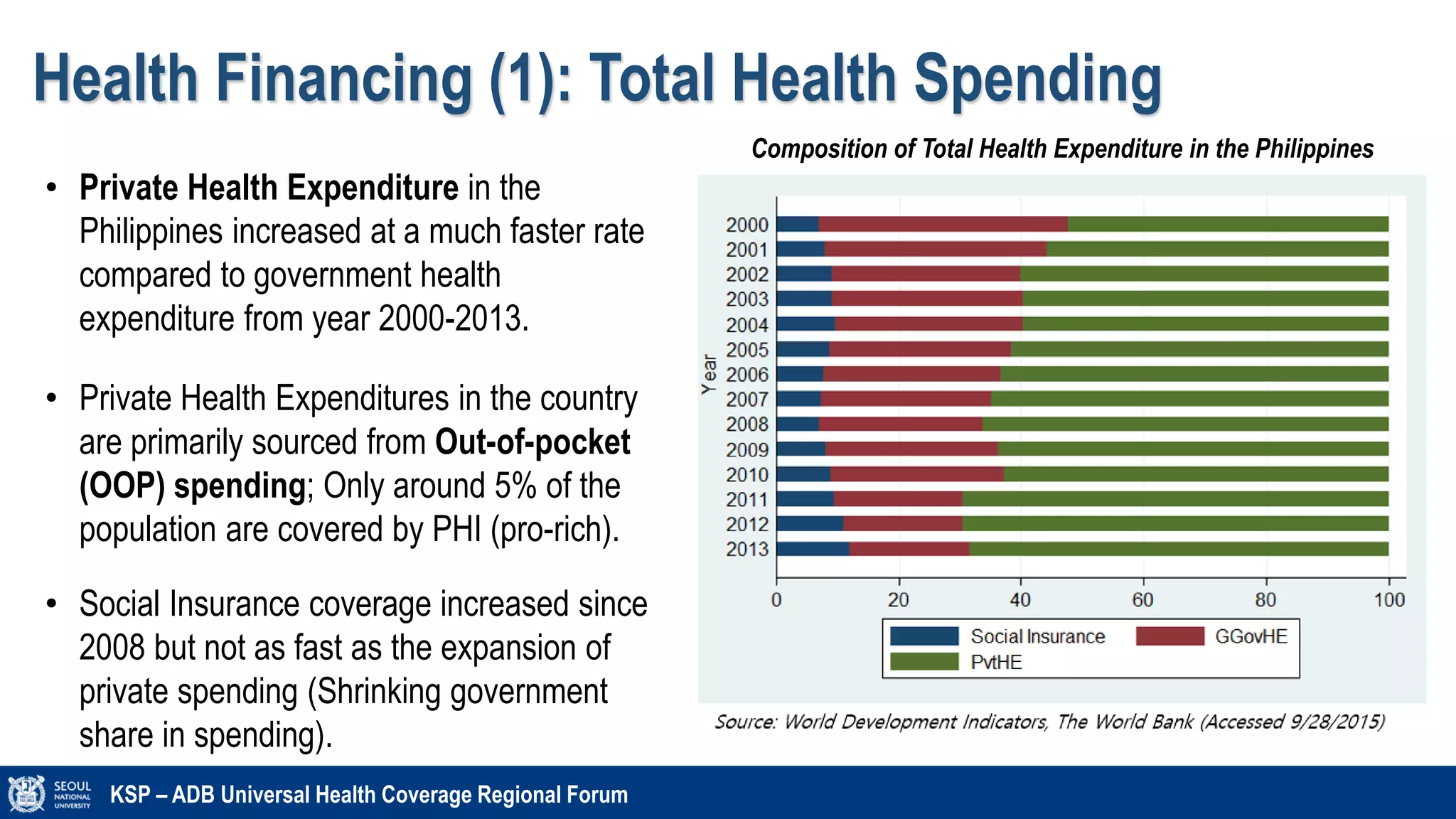
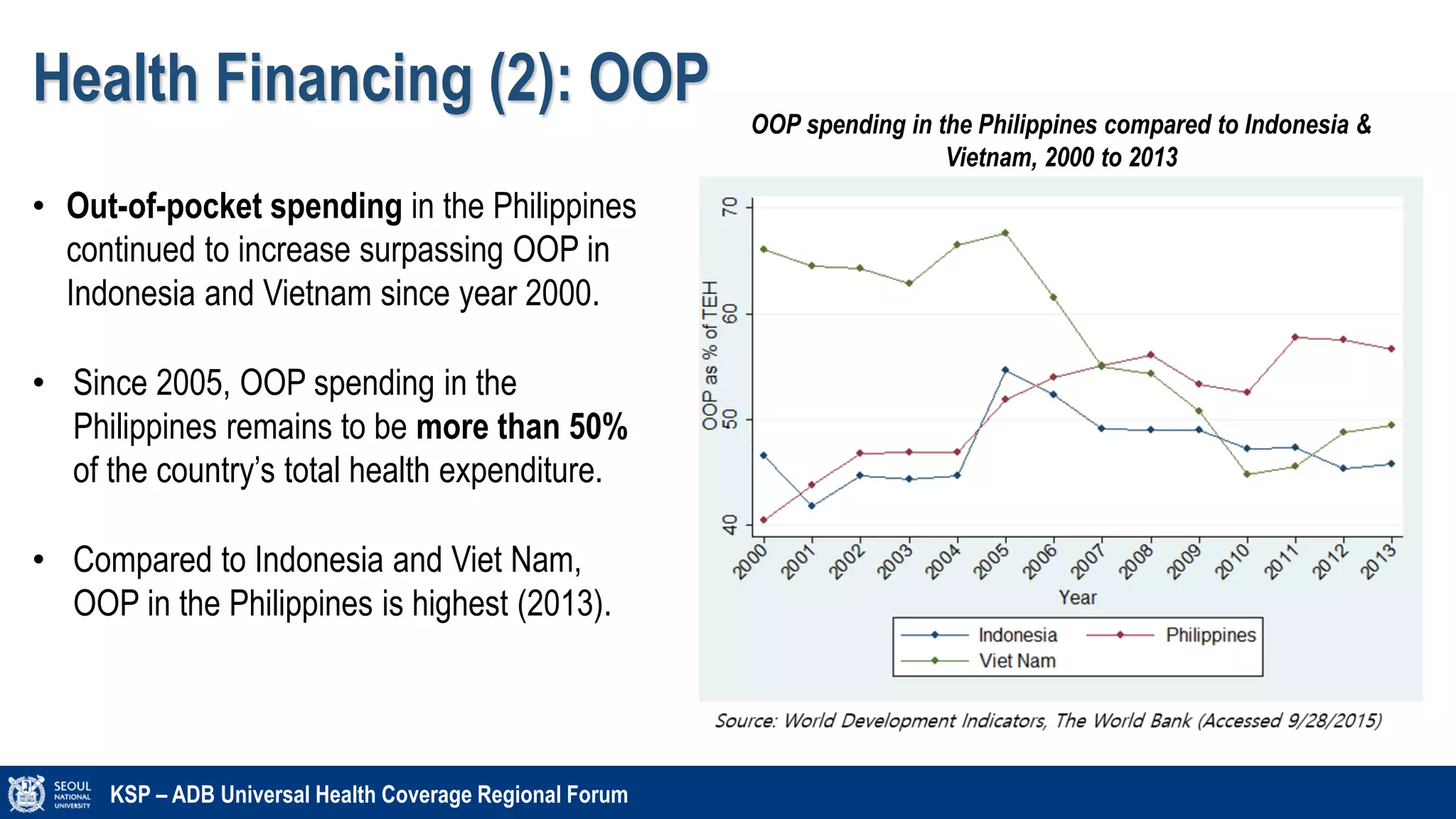
The document discusses the Philippines' health system and financing, detailing growth trends in health expenditure alongside challenges like disease transitions and out-of-pocket spending. Key reform milestones since the 1970s, such as the establishment of PhilHealth and the push for universal health coverage (UHC), are highlighted, along with strategic purchasing and payment systems for health providers. The document also emphasizes disparities in health facility distribution and coverage gaps, particularly among different income sectors.








![A. Benefit Coverage (2)
KSP – ADB Universal Health Coverage Regional Forum
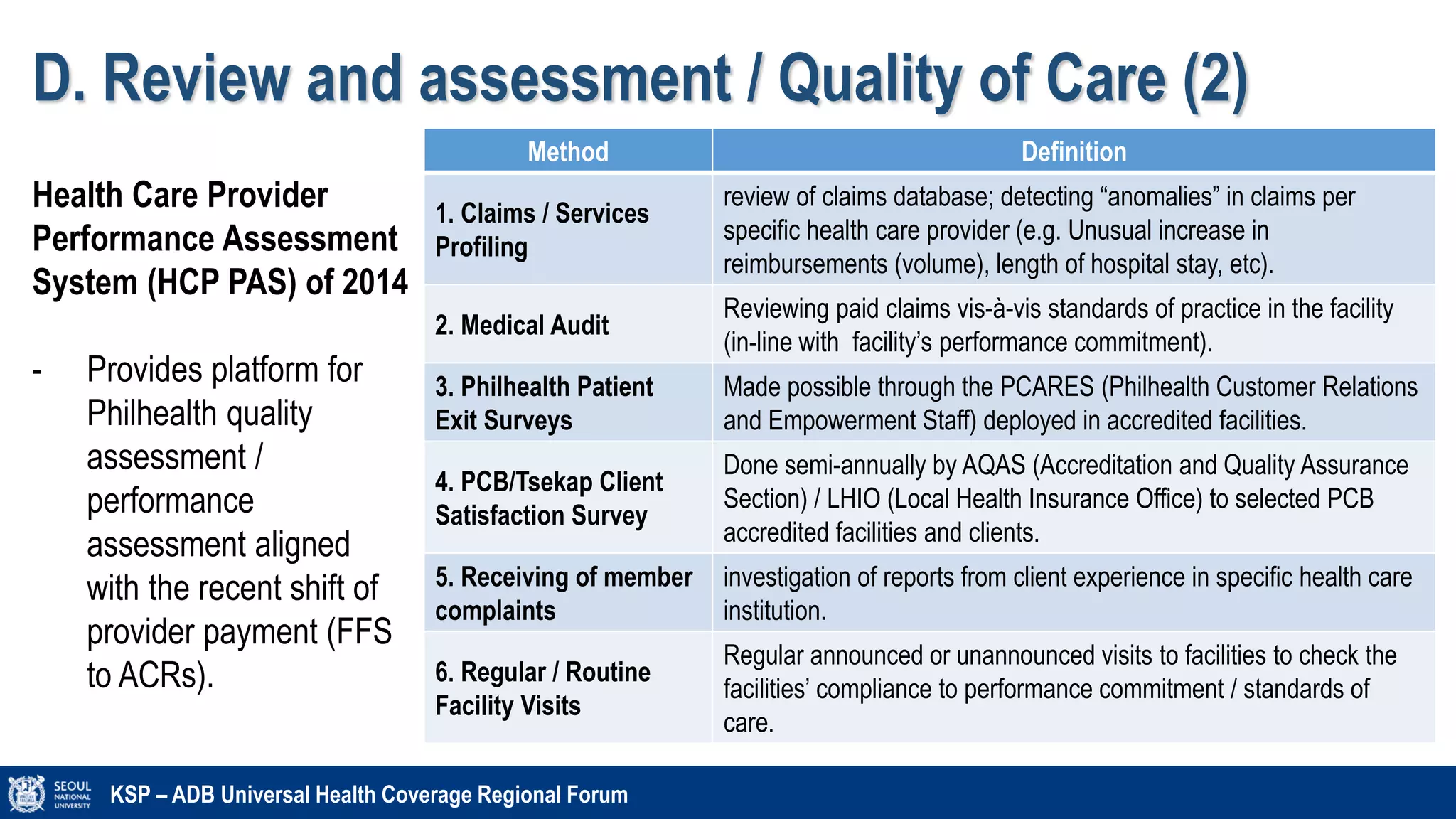
• Out-patient benefit packages are designed
per specific services provided in out-
patient facility. For example, RHUs can be
accredited in one or all of the PCB
(Tsekap), MCP, TB-DOTS, Malaria, etc.
In-
patient
benefits
• Shift from FFS to All
Care Rate (ACR)
• More pronounced
benefits (ACR)
Out-
patient
benefits
• Out-patient benefit
packages for RHUs/HCs
(OPB, MCP, TB-DOTS)
• Other OP benefits (ASC,
RT, OBT, DC)
• Other accredited out-patient services by
Philhealth includes (1) Ambulatory
Surgical Clinics (ACS) [private facilities],
(2) Dialysis centers (DC) [private & public];
Others: Outpatient blood centers and
Radiotherapy](https://image.slidesharecdn.com/philippinesksp-adb10262015-160222021258/75/Philippines-Health-system-and-Financing-2015-14-2048.jpg)