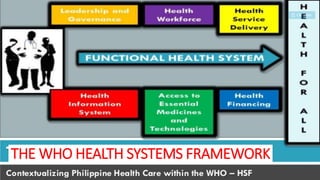
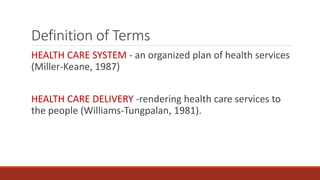
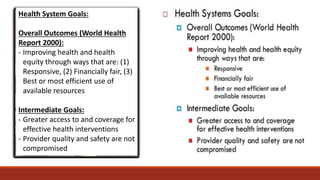
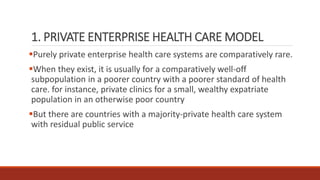
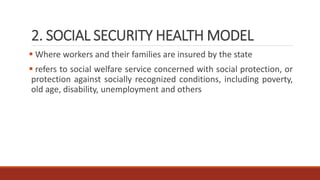
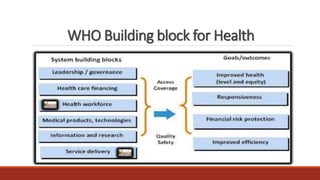
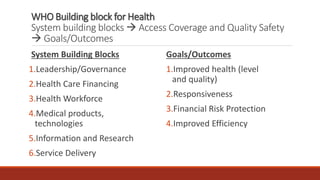
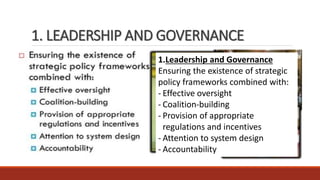
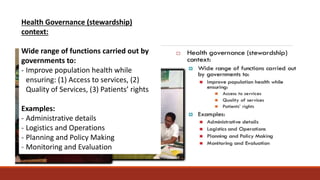
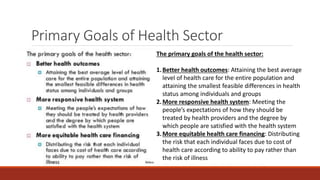
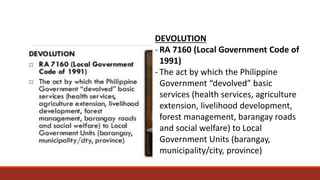
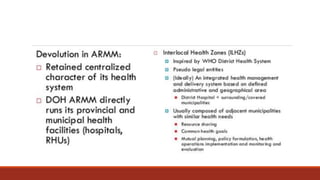
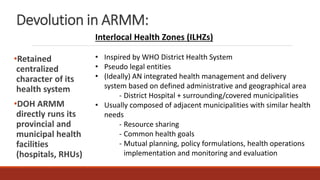
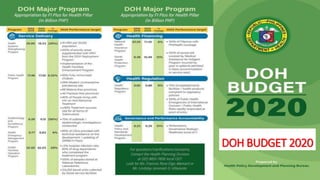
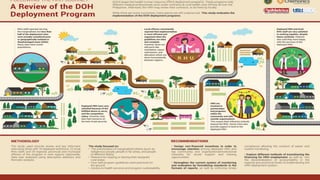
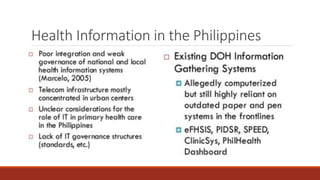
This document provides an overview of the Philippine health care system. It begins by defining key terms like health care system, health care delivery, and Philippine health care system. It then discusses the WHO health systems framework and describes the four essential functions of a health system: service provision, resource generation, financing, and stewardship. The document outlines different health care system models and describes the main components of the Philippine system, including its national health insurance program, PhilHealth. It discusses factors like leadership and governance, health care financing, the health workforce, access to medicines and technologies, health information and research, and health service delivery. Overall, the document comprehensively summarizes the organization and structure of the Philippine health care system.