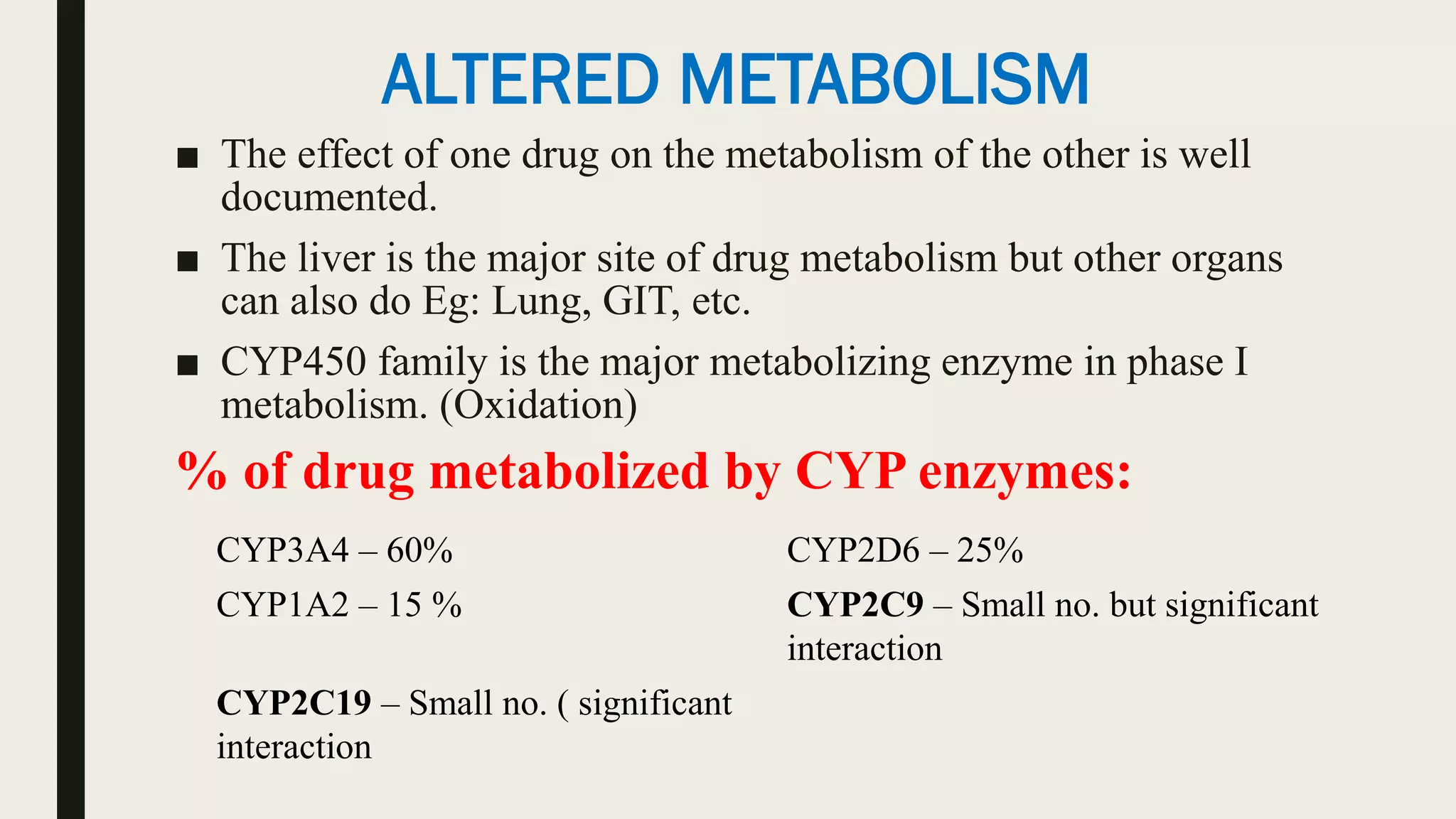
This document discusses drug interactions, their mechanisms and outcomes. It defines a drug interaction as a modification of one drug's effects due to another substance. Risks include narrow therapeutic indices, polypharmacy, multiple prescribers and patient factors. Outcomes are toxicity, therapeutic failure, beneficial effects or physical incompatibilities. Mechanisms are pharmacokinetic - affecting absorption, distribution, metabolism and excretion - or pharmacodynamic, changing receptor interactions. Specific examples are provided to illustrate different interaction types.