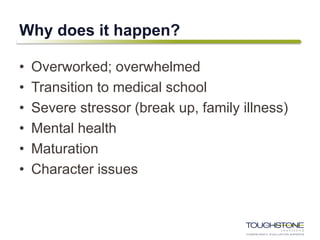
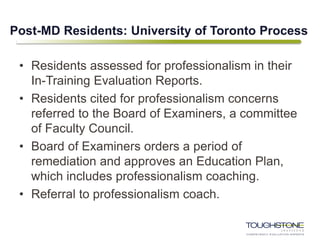
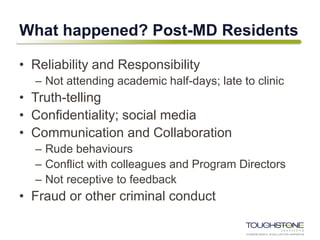
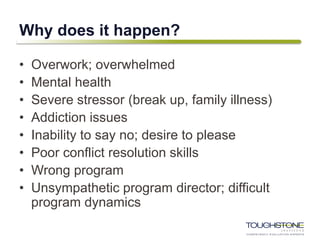
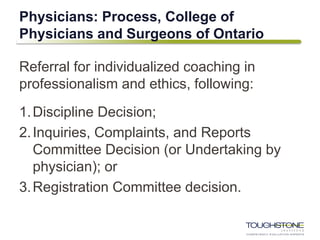
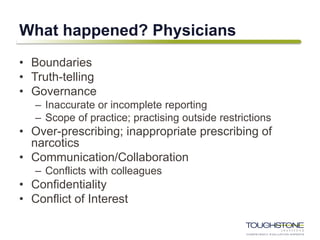
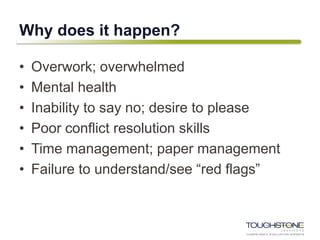
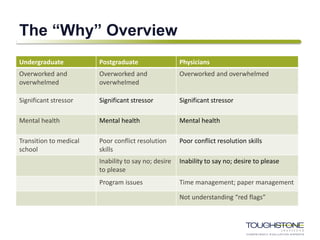
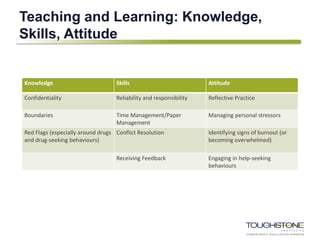
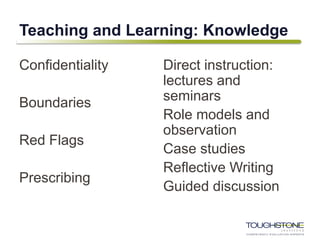
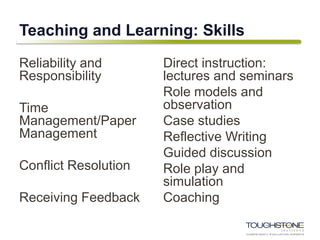
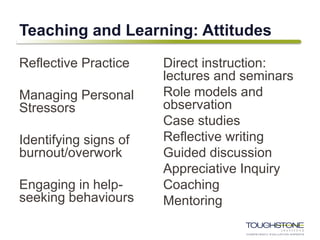
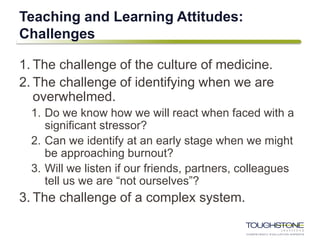
Erika Abner discussed her experience teaching professionalism to medical students, residents, and physicians through individualized instruction and coaching. She summarized common issues seen such as reliability, boundaries, and mental health. Factors contributing to lapses included stress, life events, workload, and inability to say no. Teaching strategies included direct instruction, role modeling, cases studies, and coaching skills like conflict resolution, self-care, and receiving feedback. Challenges included identifying one's limits and the medical culture. System-level responses are needed like promoting wellness and compassionate regulation. Focusing on "why" issues occur, finding balance, and supporting wellness programs can help address professionalism lapses.


![“Rather than searching for a system to find the “bad
apples,” should we view the problem from an
alternative standpoint, where any professional, when
challenged by life events, has the potential of losing
his or her way and putting patients and colleagues at
unnecessary risk?”
[Murphy, 2015 at 19]](https://image.slidesharecdn.com/erikaabner-190301142352/85/Perspectives-2019-Erika-Abner-5-320.jpg)
![Professionalism Frameworks
1. Virtues-based
– Able to apply ethical reasoning, restrain self-interest, and
demonstrate compassion and respect as a humane person.
2. Competency
– A domain of competence (behaviours) to be mastered,
demonstrated and assessed.
3. Identity formation
– Socialization into thinking, acting, and feeling like a professional.
[Irby, 2016 at 1606]
4. Social control
– Medicine’s promise to police itself in the public interest.
– Individual ability and willingness to self-regulate in the public
interest. [Hafferty, 2009 at 62]](https://image.slidesharecdn.com/erikaabner-190301142352/85/Perspectives-2019-Erika-Abner-7-320.jpg)
![Teaching and Learning [Irby, 2016 at 1609]
Strategies Virtue-based Behavior-based Professional identity
Pedagogy Direct instruction, role
models, case studies,
reflective writing, guided
discussion, appreciative
inquiry, white coat
ceremonies
Direct instruction, role
models, case studies,
coaching, simulations,
reflection on action
Direct instruction, role
models, case studies,
reflective writing, guided
discussion, appreciative
inquiry](https://image.slidesharecdn.com/erikaabner-190301142352/85/Perspectives-2019-Erika-Abner-8-320.jpg)
![Shifting to thinking about the system….
“Burnout is primarily a system-level problem
driven by excess job demands and
inadequate resources and support, not an
individual problem triggered by personal
limitations.” [Shanafelt et al at 1828]](https://image.slidesharecdn.com/erikaabner-190301142352/85/Perspectives-2019-Erika-Abner-25-320.jpg)
![System-level Responses
Canadian Medical Protective
Association
1. Medical Schools should develop a
culture of wellness.
2. Medical organizations should look
for ways to assist physicians.
3. Medical regulators should aim for
“compassionate regulation.”
4. Institutional and hospital leaders
should recognize the business
case.
5. Governments should invest in
physician wellness. [CMPA 2018]
Federation of State Medical Boards
[US]
1. State medical boards should
emphasize the importance of
physician health, self-care, and
treatment-seeking….
2. Professional medical societies have
a key role in encouraging physicians
to seek treatment….
3. Centers for Medicaid and Medicare
services should carefully analyze
any new requirements placed on
physicians to determine their
potential impact on physician
wellness.
4. Medical schools and residency
programs should continue to
improve the culture of medicine.
[FSMB Workgroup 2018 Report,
selected recommendations]](https://image.slidesharecdn.com/erikaabner-190301142352/85/Perspectives-2019-Erika-Abner-26-320.jpg)