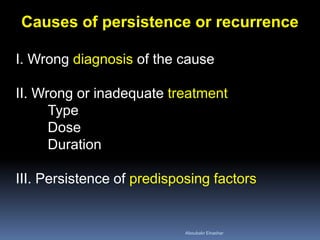
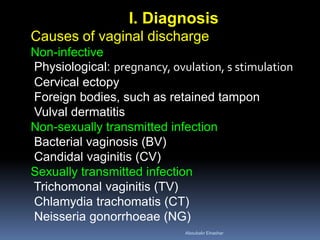
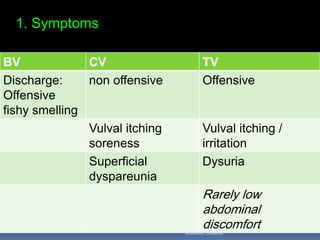
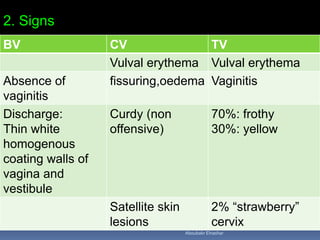
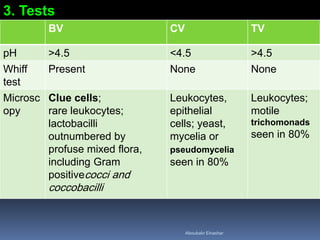
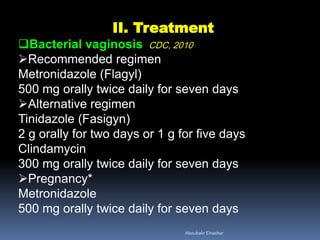
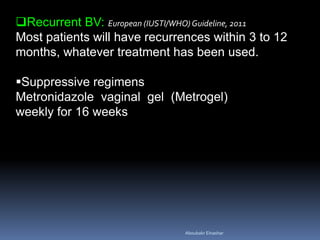
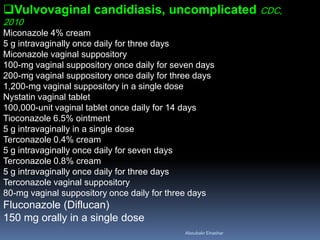
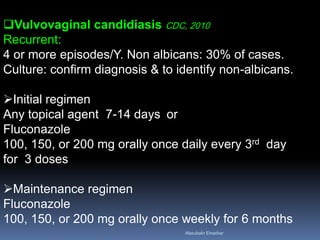
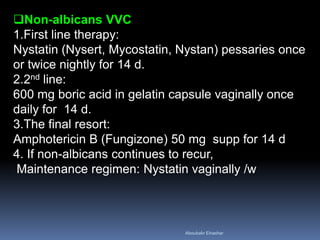
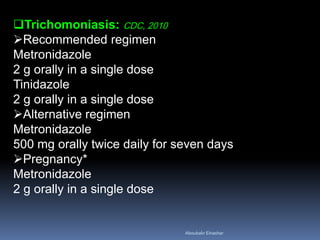
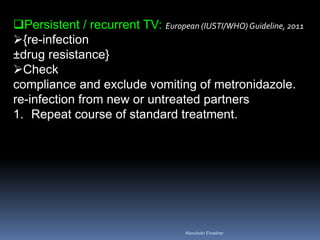
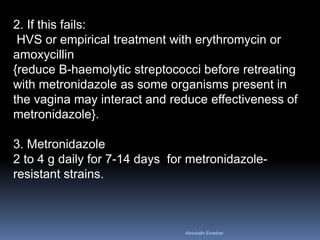
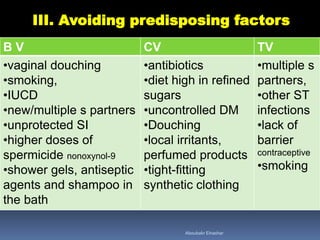
This document discusses the causes, diagnosis, and treatment of persistent or recurrent vaginal discharge. It outlines various infectious and non-infectious causes including bacterial vaginosis, candidal vaginitis, and trichomonal vaginitis. The document provides details on symptoms, signs, and tests for diagnosis. It recommends treatments for each condition such as oral and topical antifungal and antibiotic regimens. Factors that can predispose women to recurrent infections are also identified, including multiple sexual partners, STIs, and lack of barrier contraception.