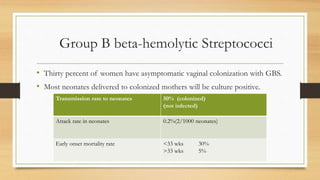
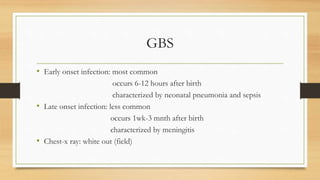
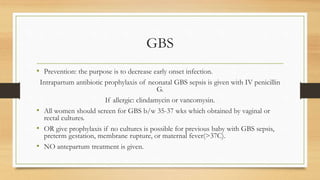
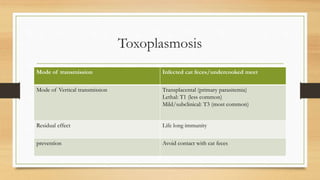
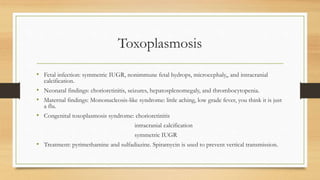
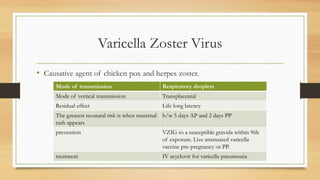
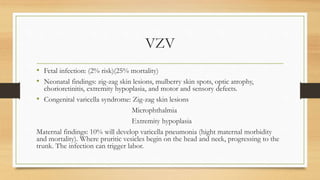
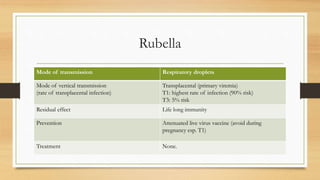
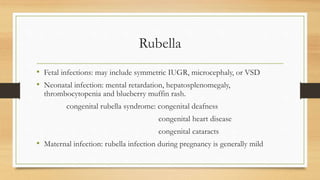
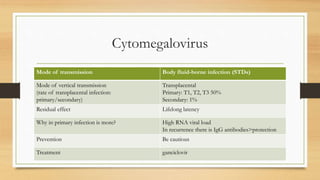
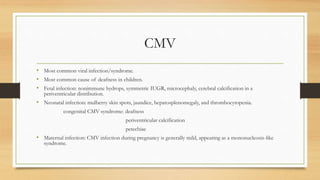
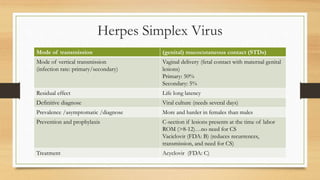
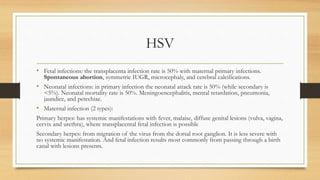
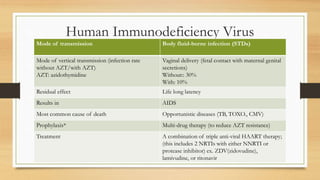
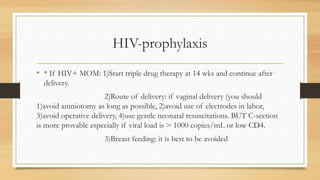
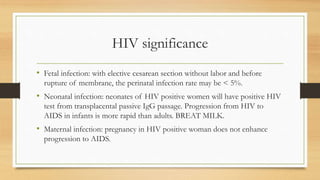
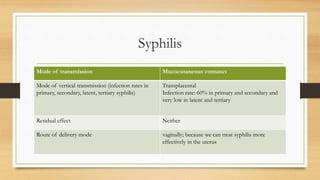
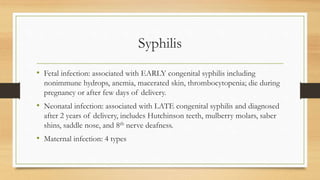
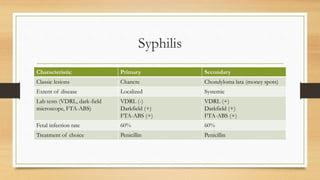
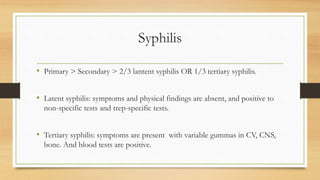
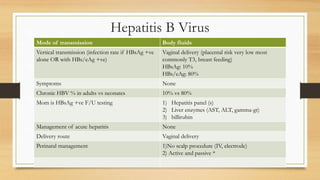
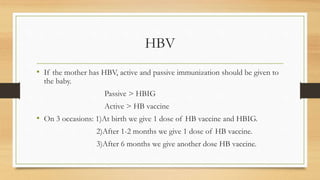
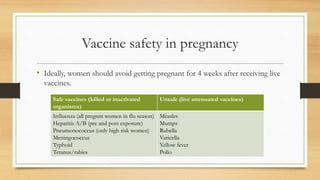
Perinatal infections can cause serious complications in neonates if transmitted from mother to fetus during pregnancy or delivery. The document discusses several important perinatal infections including GBS, toxoplasmosis, rubella, CMV, HSV, HIV, syphilis, and HBV. For each infection, it summarizes the mode of transmission, risk of vertical transmission, potential fetal and neonatal effects, and recommendations for prevention and treatment.