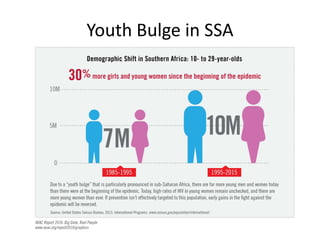
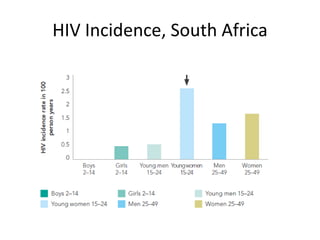
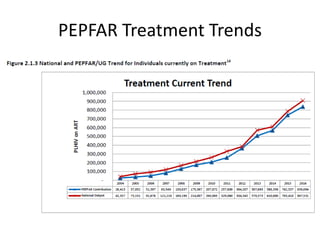
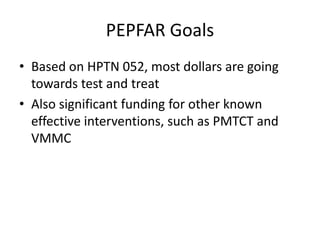
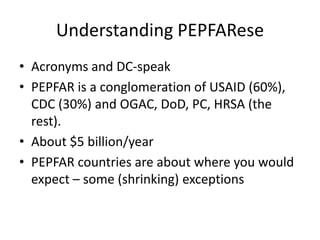
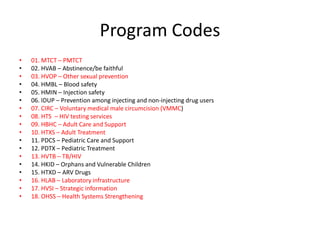
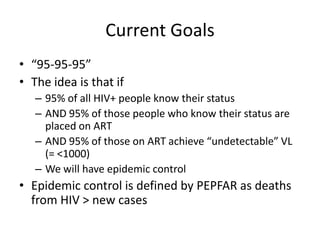
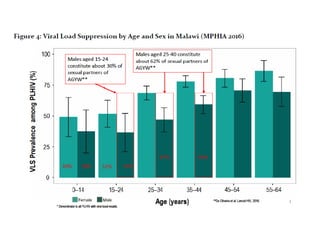
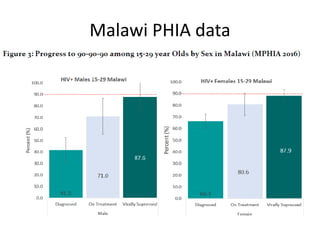
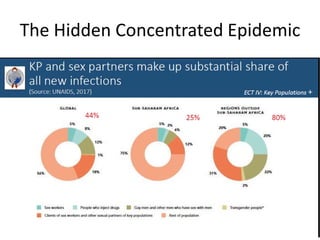
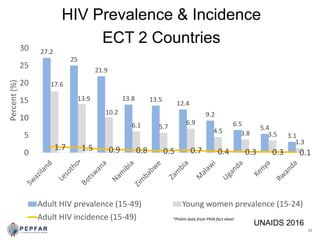
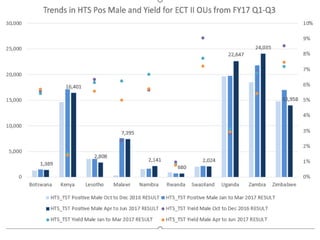
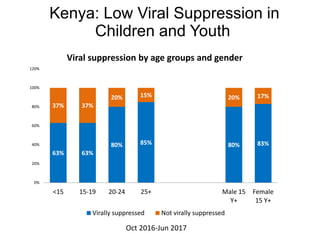
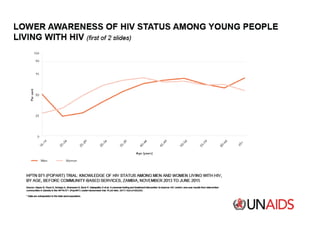
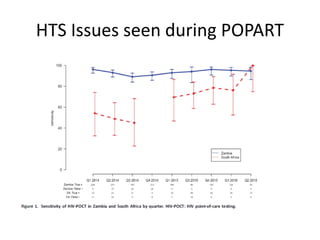
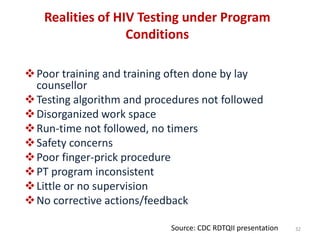
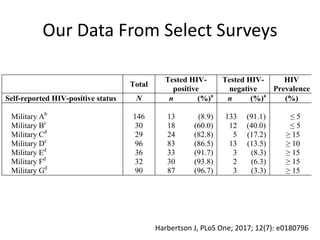
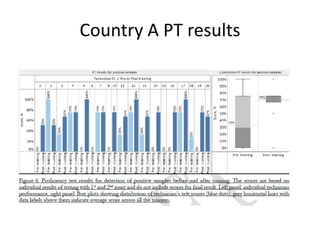
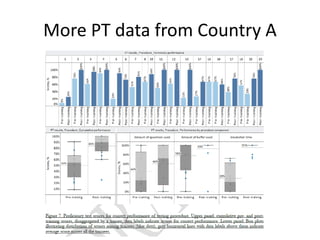
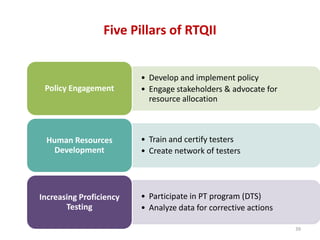
This document provides an overview of the President's Emergency Plan for AIDS Relief (PEPFAR) program, including its goals, strategies, and challenges. PEPFAR aims to control the HIV/AIDS epidemic through strategies like testing and treatment (95-95-95 goals), focusing on high-risk populations and geographic hotspots, and strengthening HIV testing services. However, PEPFAR faces ongoing challenges like ensuring accurate HIV testing and achieving viral suppression targets among youth. The document discusses ongoing efforts to address weaknesses in HIV testing practices and increase testing quality through proficiency testing, monitoring, and training.