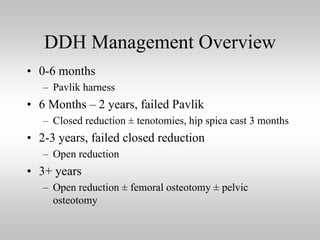
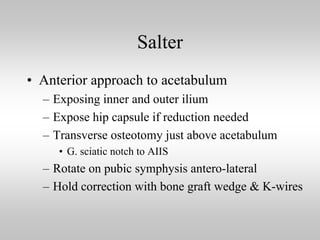
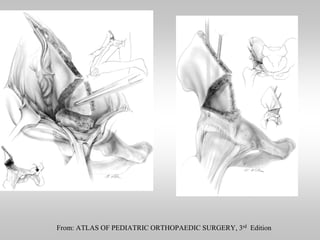
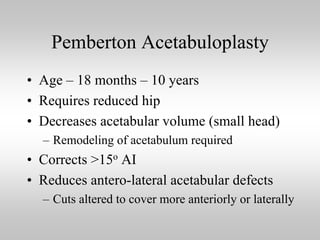
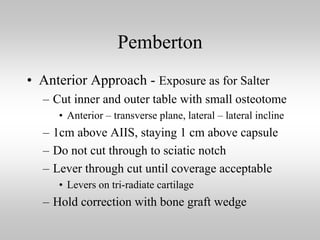
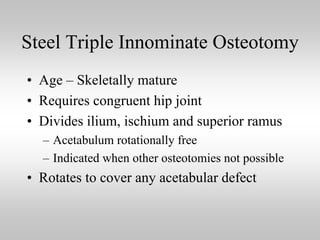
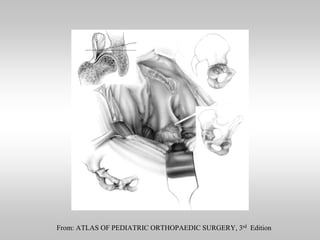
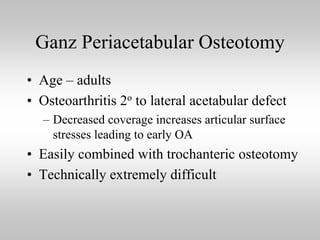
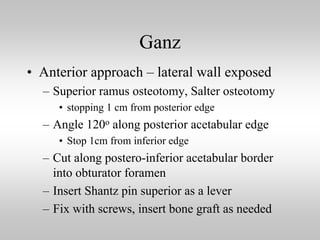
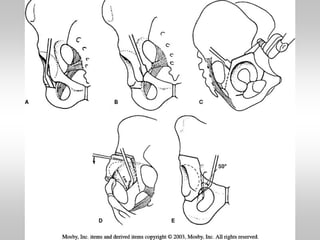
This document discusses several types of pelvic osteotomies used to treat developmental dysplasia of the hip. The main osteotomies covered are the Salter single innominate osteotomy, Pemberton acetabuloplasty, Steel triple innominate osteotomy, Chiari medial displacement, and Ganz periacetabular osteotomy. Most pelvic osteotomies require remodeling of the bone and are not as useful in older children over age 8. Careful matching of the procedure to each patient's individual case is needed. The more complex osteotomies have a steep learning curve for surgeons.