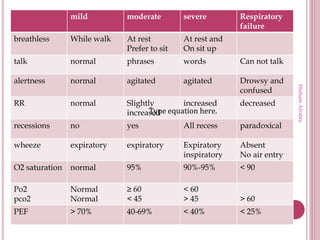
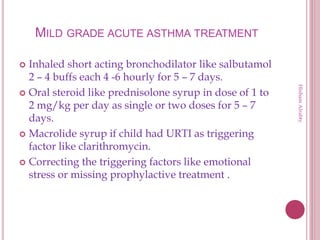
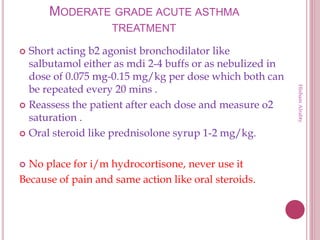
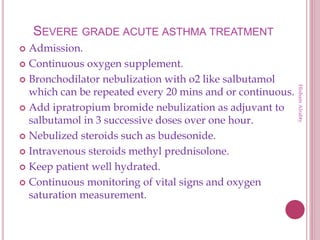
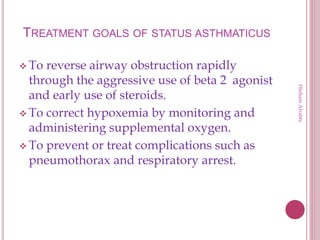
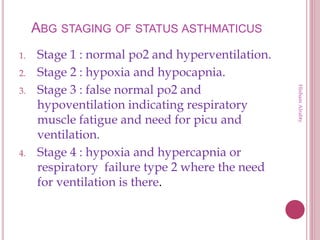
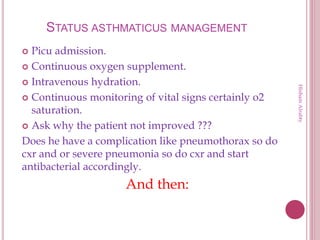
This document provides definitions and classifications for acute asthma attacks and outlines treatment protocols based on severity. It defines mild, moderate, and severe acute asthma and describes recommended treatments including bronchodilators, steroids, magnesium sulfate, and ventilation. It also discusses treatments for status asthmaticus, including various bronchodilators, steroids, and ventilation strategies.