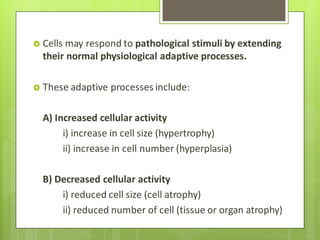
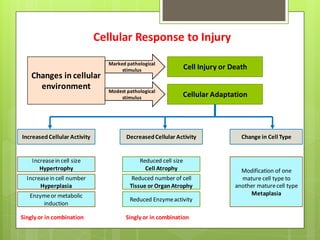
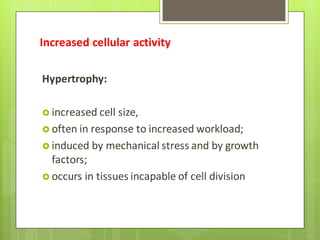
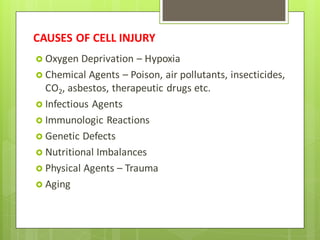
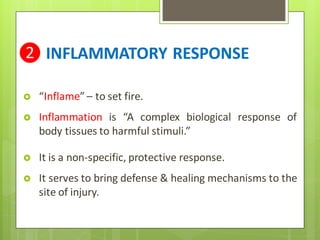
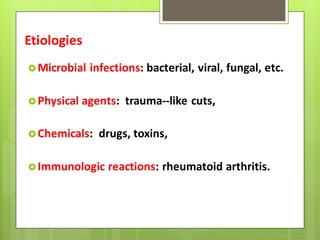
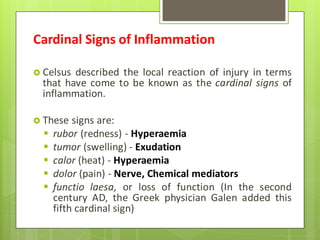
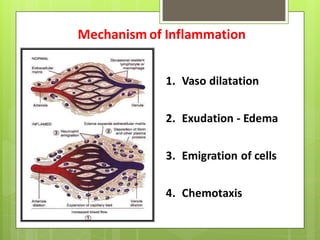
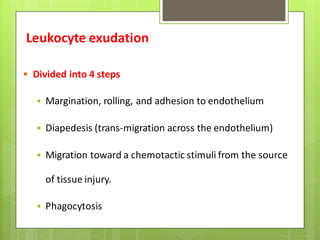
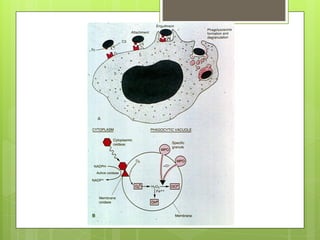
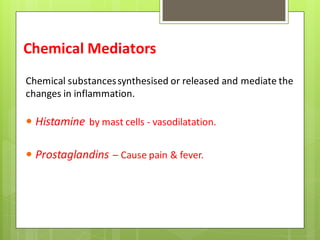
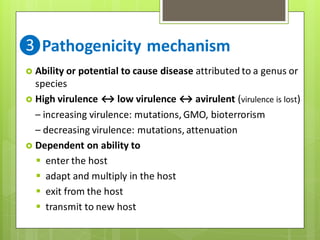
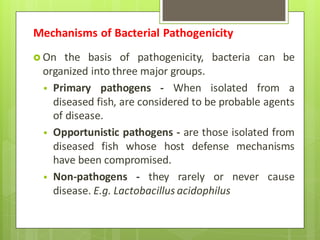
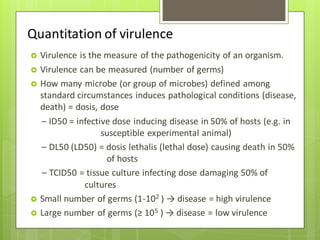
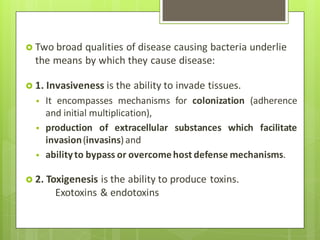
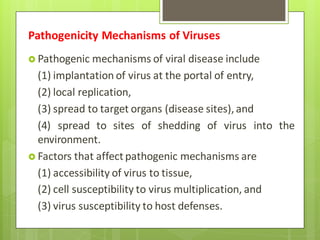
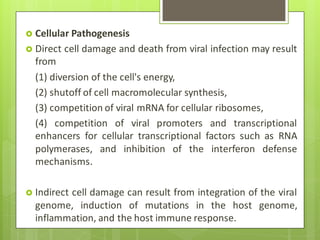
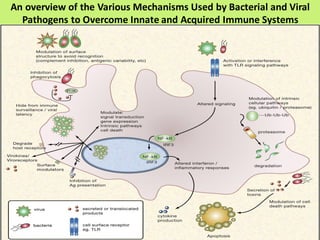
The document details the complex process of disease development in aquaculture, emphasizing the roles of various pathogens and environmental factors in pathology. It outlines cellular responses to injury, the inflammatory response to harmful stimuli, and the pathogenicity mechanisms of bacteria, viruses, parasites, and fungi. Understanding these processes is essential for addressing disease in aquatic organisms and involves investigating interactions between pathogens and host defenses.