1) Anti-Müllerian hormone (AMH) is produced by granulosa cells and reflects the ovarian follicle pool, making it a useful marker of ovarian reserve that is not affected by hormones or the menstrual cycle.
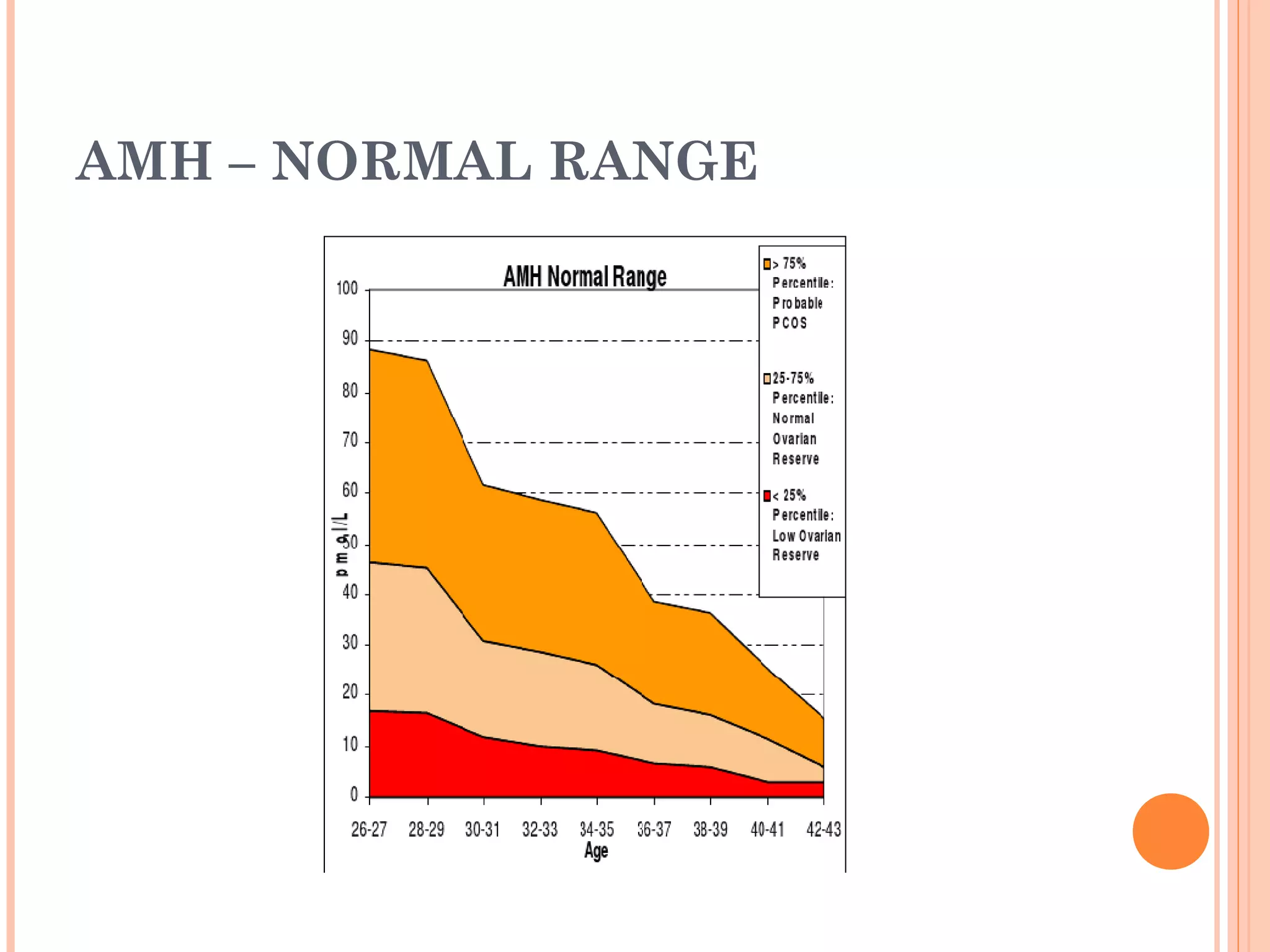
2) AMH levels decline with age in a predictable pattern and lower levels predict a poorer response to fertility treatments, while higher levels indicate greater risk of ovarian hyperstimulation syndrome.
3) AMH alone or in combination with antral follicle count is currently the best assessment of ovarian reserve compared to other hormonal or ultrasound markers. AMH can predict both poor and excessive responses to fertility medication.