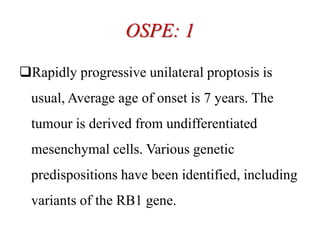
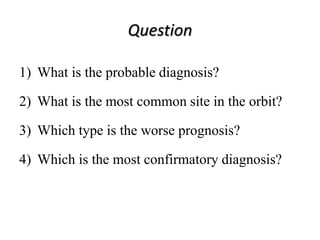
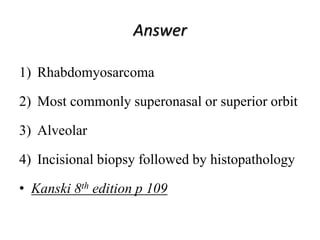
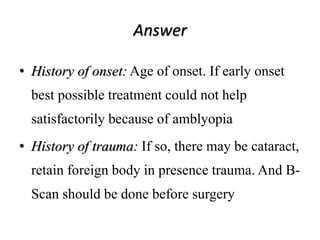
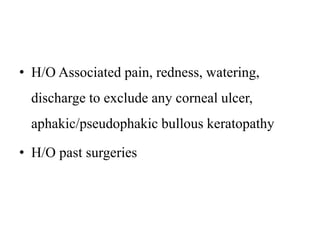
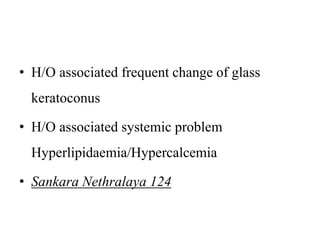
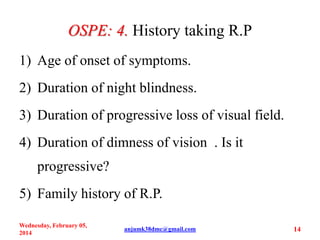
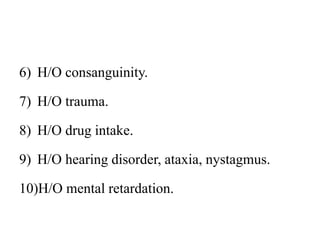
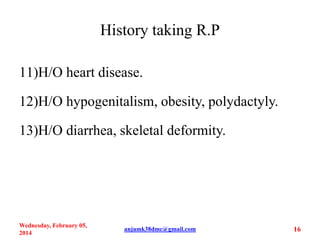
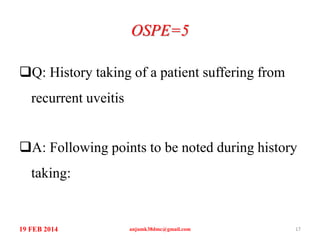
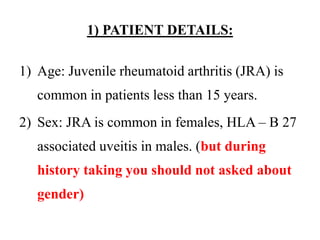
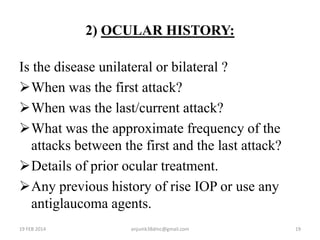
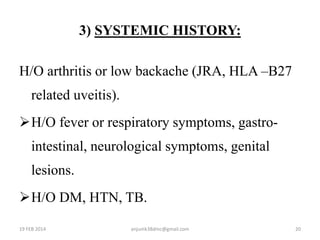
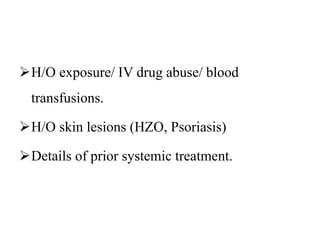
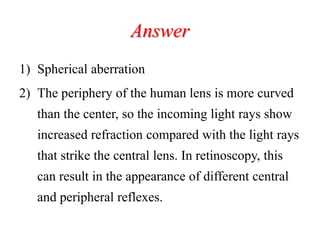
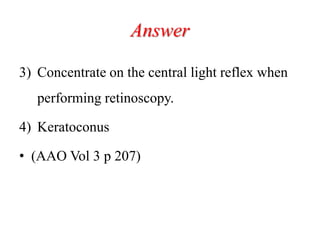
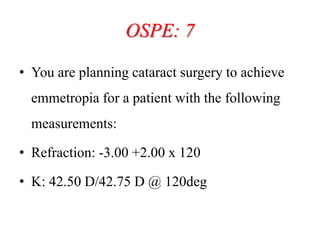
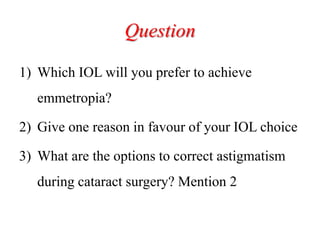
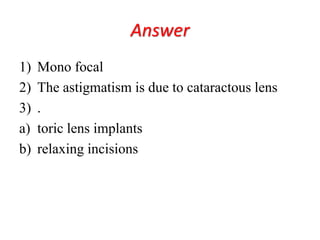
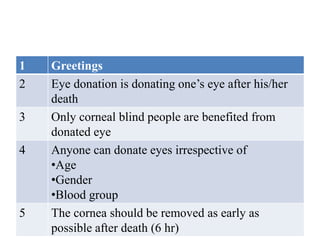
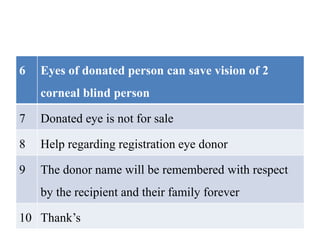
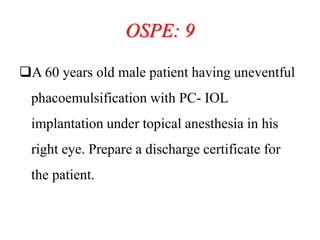
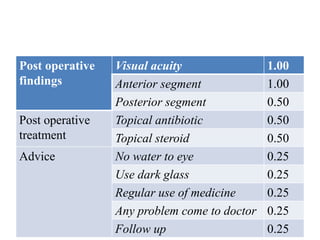
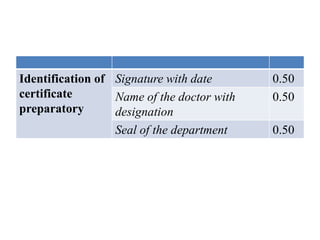
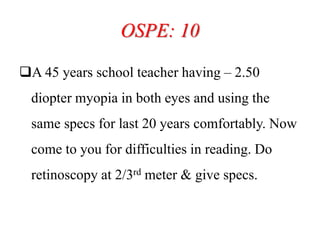
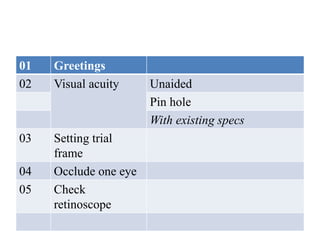
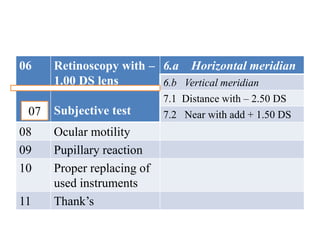
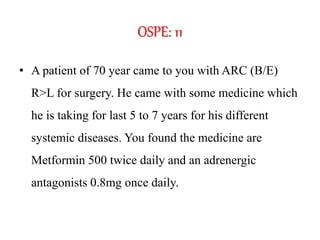
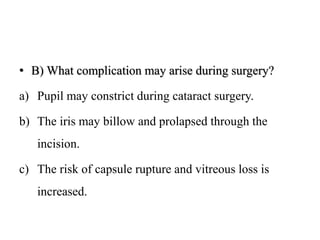
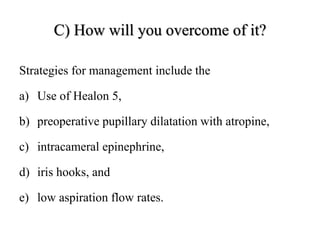
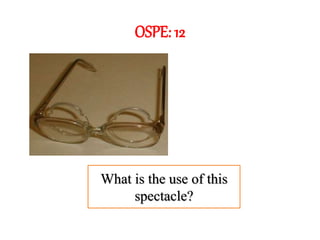
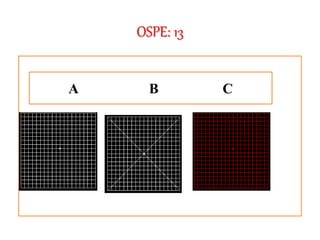
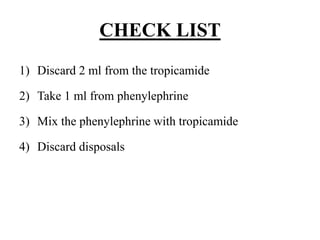
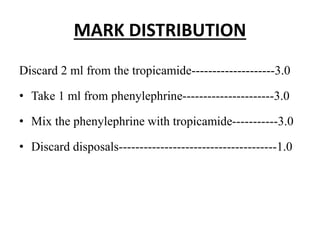
The document outlines various examination procedures and assessments for ocular conditions, including diagnosing rhabdomyosarcoma, performing the Schirmer test, and taking patient histories related to corneal opacities and recurrent uveitis. It also covers practical examination techniques such as retinoscopy and cataract surgery preparations, along with the importance of eye donation. Specific case examples illustrate the interpretation of test results, necessary preoperative precautions, and management strategies for different ophthalmic conditions.