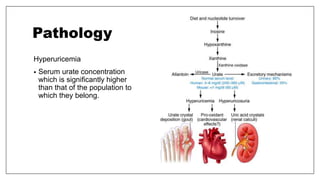
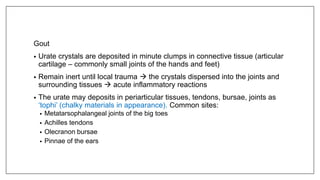
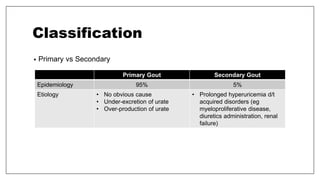
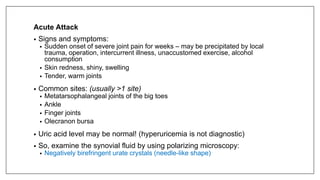
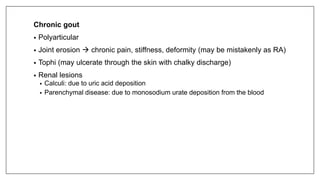
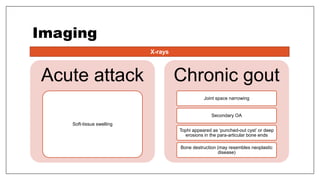
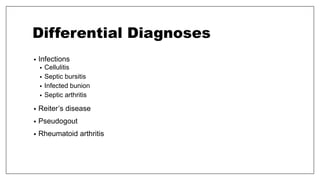
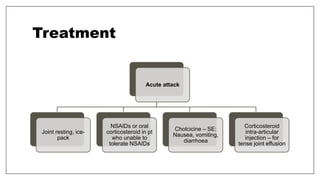
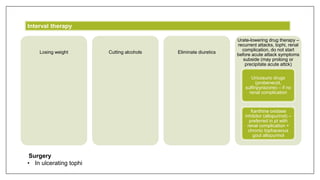
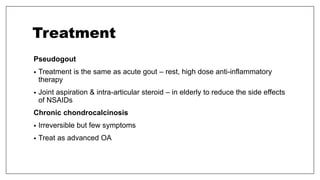
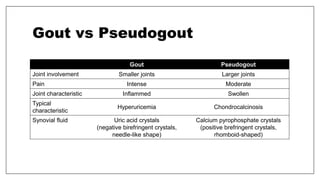
The document discusses crystal deposition disorders affecting joints, primarily focusing on gout and pseudogout. It outlines the causes, clinical features, diagnostic methods, and treatment options for both conditions, emphasizing the differences between them in terms of joint involvement and crystal types. Additionally, it highlights the importance of understanding hyperuricemia and its role in gout pathogenesis, as well as the treatment strategies for managing acute and chronic symptoms.