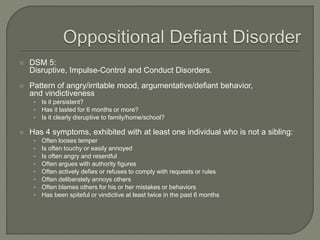
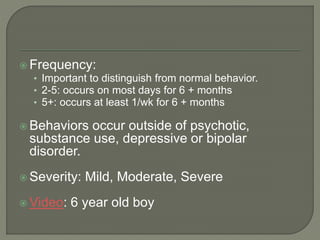
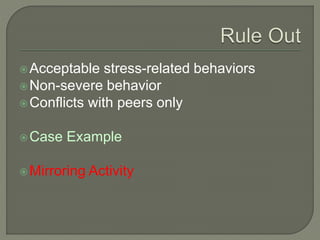
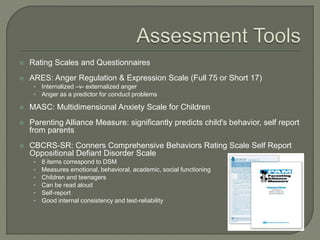
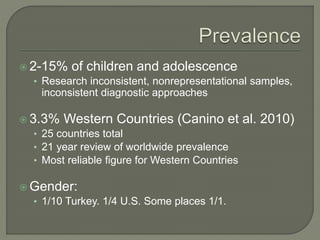
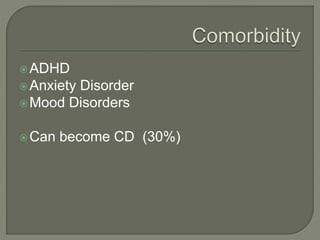
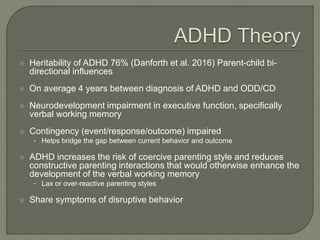
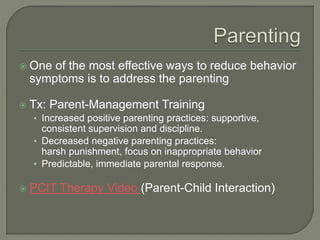
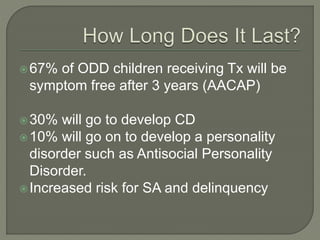
The document summarizes Oppositional Defiant Disorder (ODD), including its diagnostic criteria, prevalence rates, common behaviors, risk factors, treatment approaches, and prognosis. ODD is characterized by angry, irritable mood and argumentative/defiant behavior lasting at least 6 months. Parent-management training to improve positive parenting strategies and reduce negative ones is considered one of the most effective treatment approaches. Approximately two-thirds of children with ODD receiving treatment will be symptom-free after 3 years.