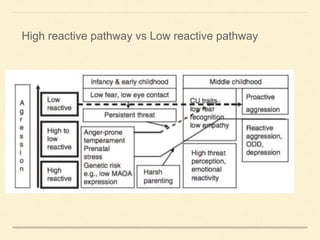
1. Disruptive disorders like oppositional defiant disorder and conduct disorder affect 5-10% of children and can persist into adulthood if left untreated.
2. They are characterized by angry, defiant, or vindictive behaviors in the case of ODD and aggression, destruction of property, deceitfulness or theft for conduct disorder.
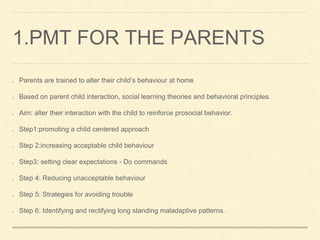
3. Early intervention with parenting skills training and social skills training for children can help alter coercive family processes and problematic parenting practices that perpetuate disruptive behaviors. Treatment aims to improve the child's behavior at home and school through reinforcement of prosocial skills.