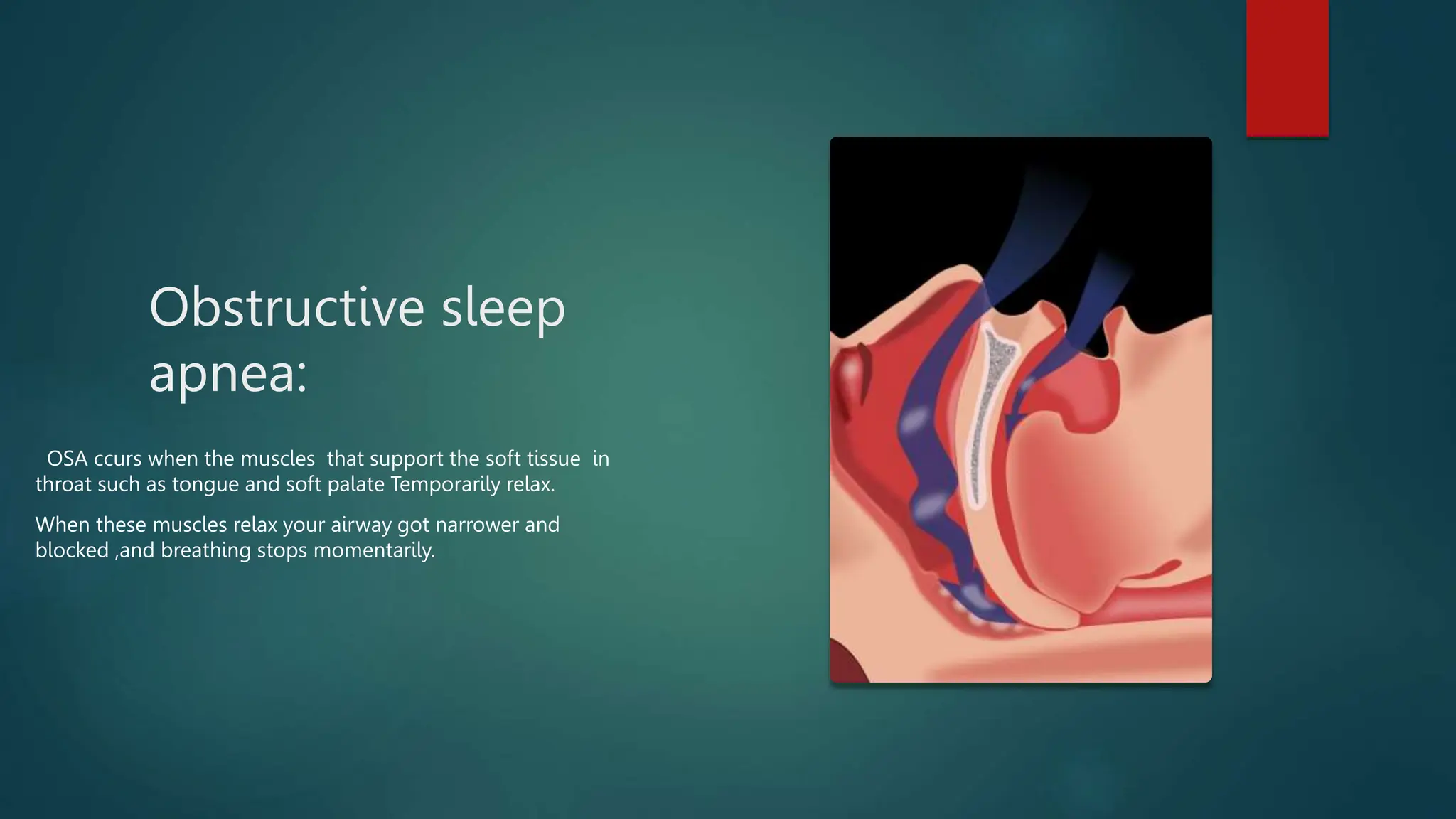
The document presents an overview of obstructive sleep apnea (OSA) and obesity hypoventilation syndrome (OHS), including definitions, risk factors, clinical features, diagnosis, and treatment options. OSA is characterized by breathing interruptions during sleep due to upper airway obstruction, while OHS is related to insufficient breathing in overweight individuals leading to oxygen and carbon dioxide imbalances. Treatment approaches for both conditions include lifestyle changes, physical interventions, and, in some cases, surgery.