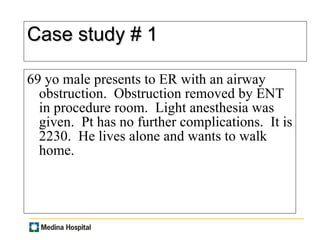
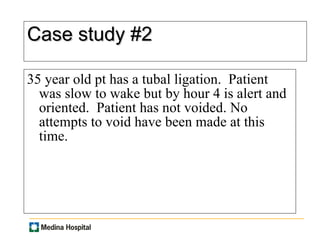
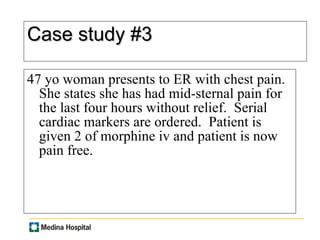
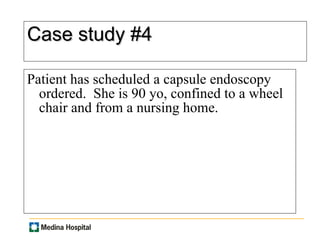
This document provides information about observation status in a hospital setting. It defines observation as allowing a physician time to determine the most appropriate care setting for a patient within 23 hours. Severity of illness refers to a patient's clinical symptoms, while intensity of service means interventions ordered by a physician to treat the patient. Some examples that may warrant observation are complications from surgery like bleeding or inability to void, as well as medical issues like chest pain or nausea. Proper documentation of an observation order is required for every observation patient. Several case studies are presented to demonstrate potential observation scenarios.