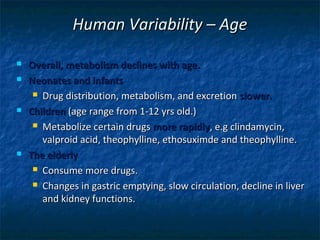
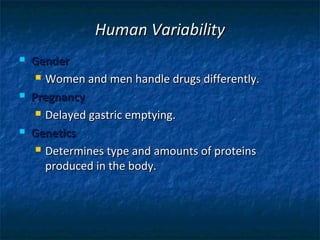
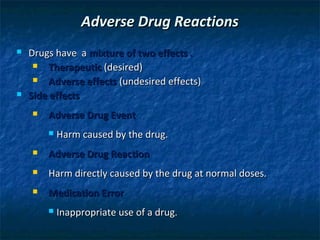
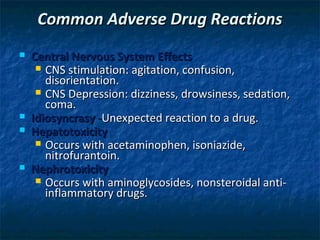
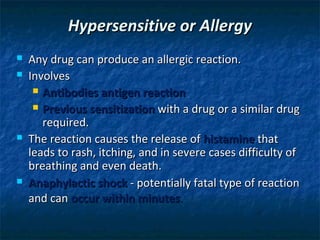
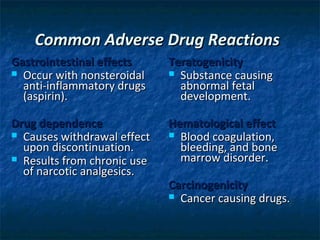
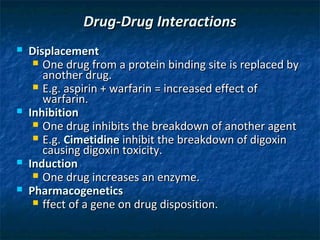
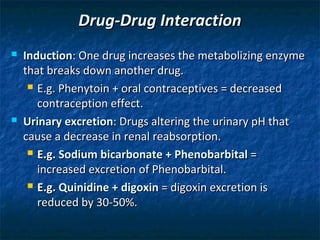
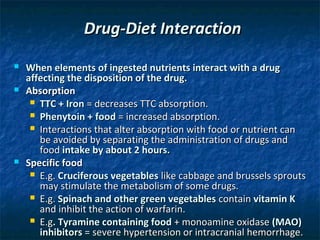
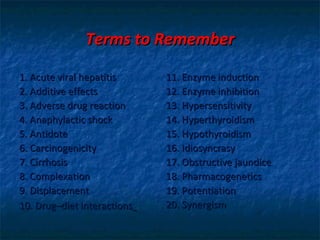
This chapter discusses factors that affect drug activity, including human variability, disease states, adverse drug reactions, drug-drug interactions, and drug-diet interactions. It covers how factors like age, gender, genetics, weight, diseases, and food can impact drug metabolism and effects in the body. Specific drug interaction topics covered are additive effects, potentiation, synergism, antidotes, enzyme induction/inhibition, and displacement interactions. Key terms related to these concepts are also defined.