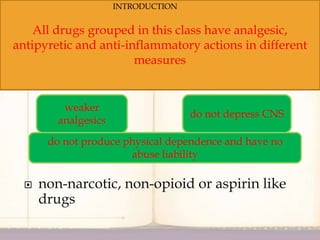
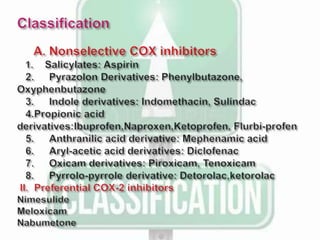
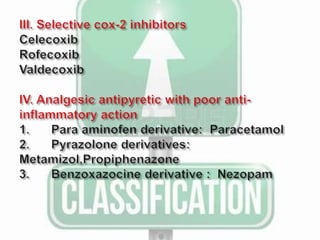
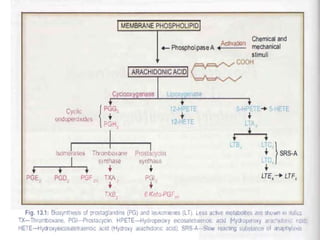
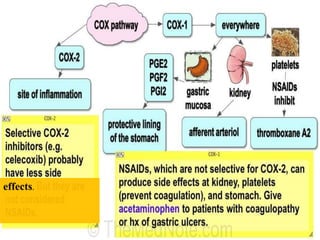
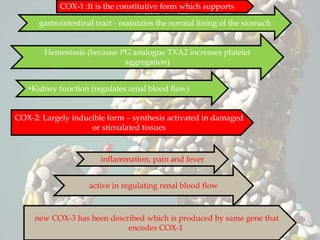
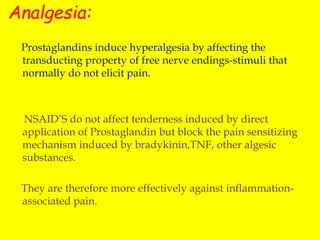
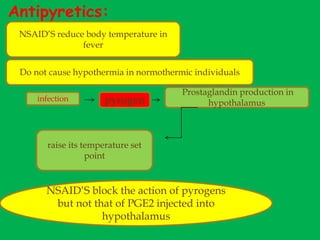
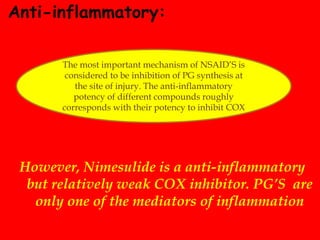
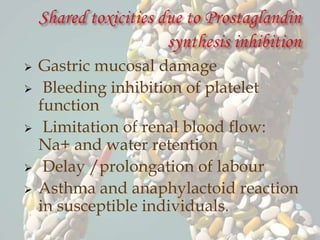
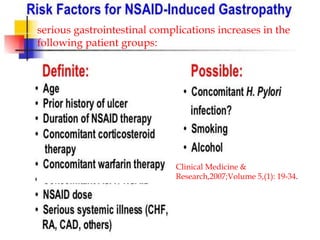
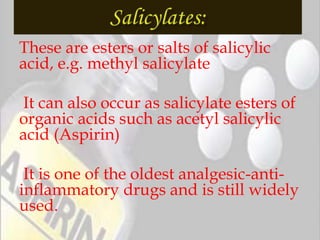
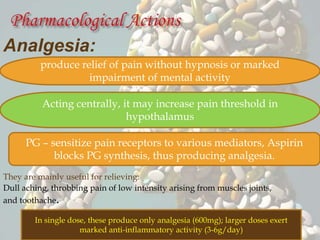
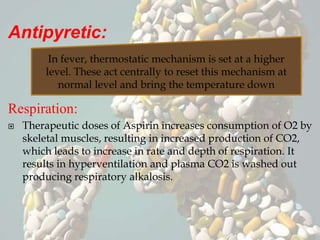
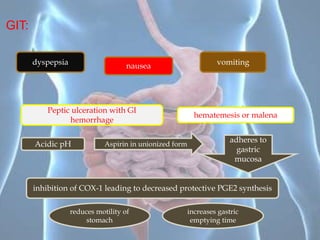
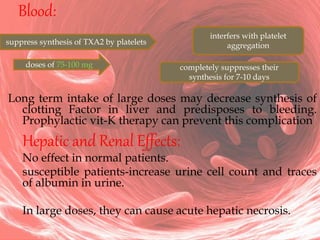
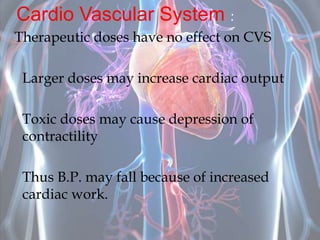
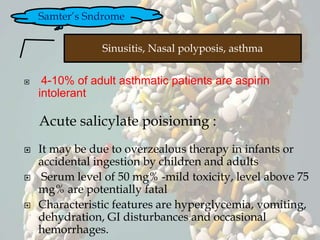
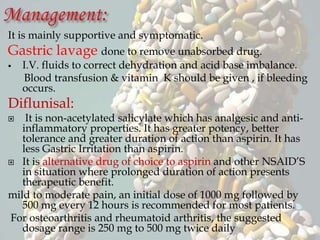
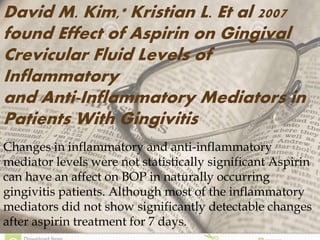
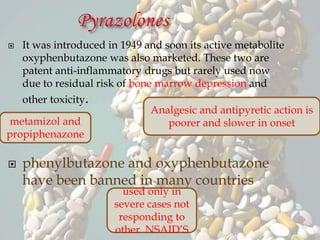
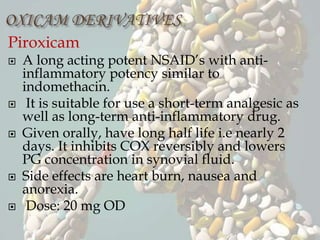
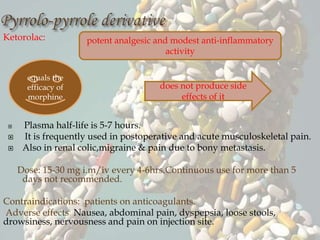
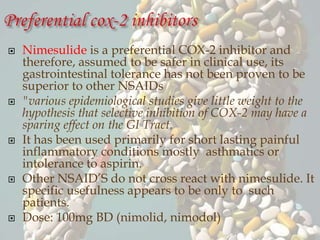
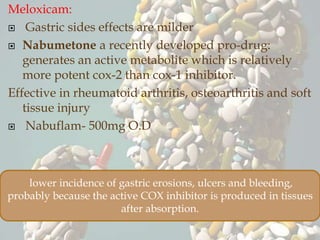
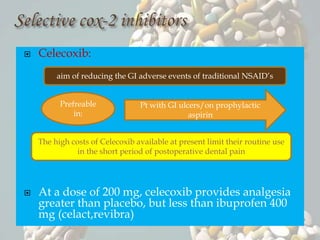
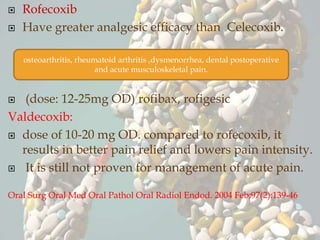
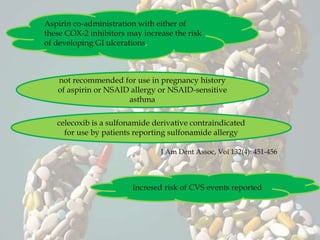
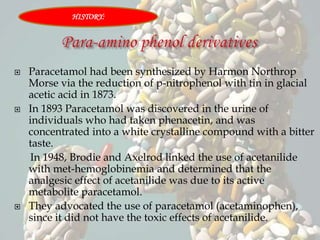
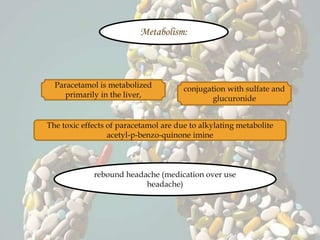
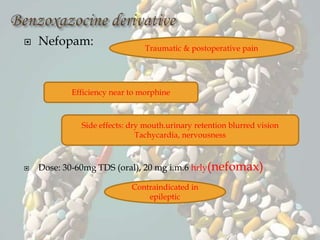
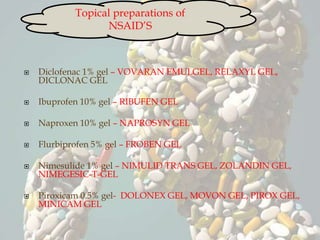
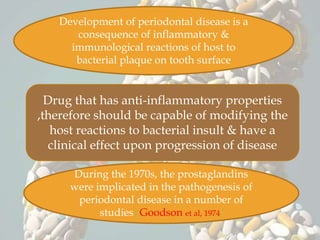
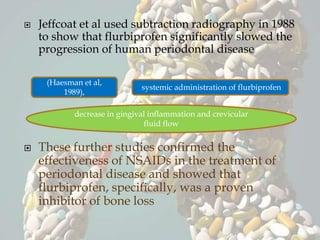
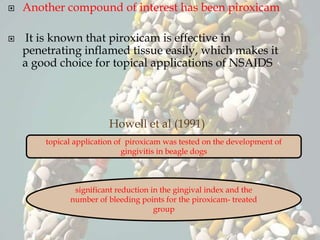
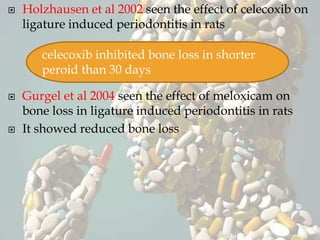
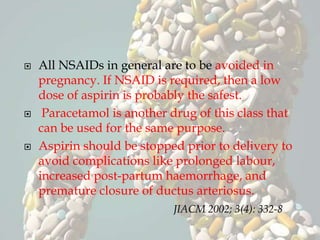
This document discusses non-steroidal anti-inflammatory drugs (NSAIDs). It covers the classification of NSAIDs, their general mechanism of action involving inhibition of cyclooxygenase (COX) enzymes, and their beneficial and risk factors. Specific NSAIDs discussed include aspirin, diflunisal, piroxicam, indomethacin, ibuprofen, ketorolac, mephenamic acid, diclofenac, and selective COX-2 inhibitors. The roles of NSAIDs in periodontics and controlling disease progression are examined. Current recommendations and the role of NSAIDs in the future are also mentioned.