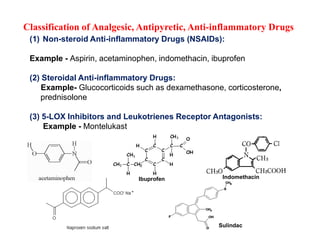
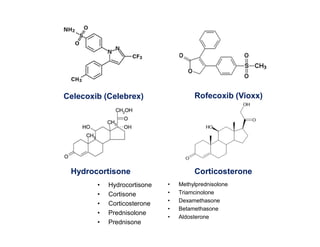
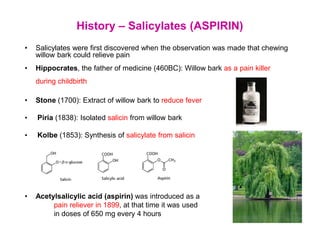
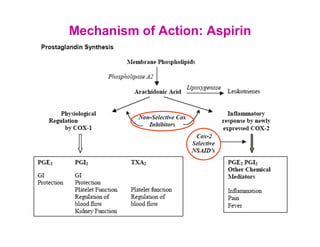
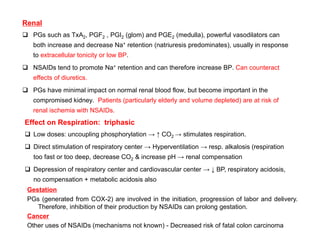
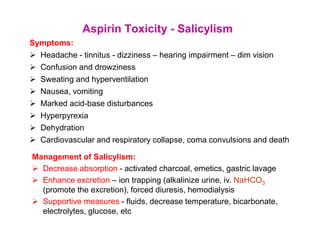
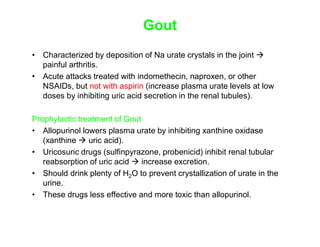
The document discusses analgesic, antipyretic, and anti-inflammatory drugs. It classifies them into three categories: (1) non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, acetaminophen, and ibuprofen; (2) steroidal anti-inflammatory drugs such as dexamethasone and prednisolone; and (3) 5-LOX inhibitors and leukotriene receptor antagonists such as montelukast. It then provides details on the mechanisms of action, pharmacological effects, therapeutic uses, and toxicity of aspirin.