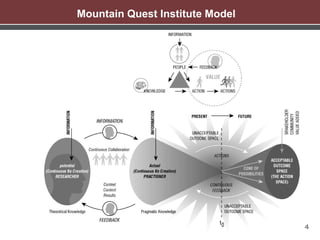
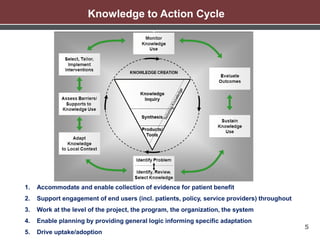
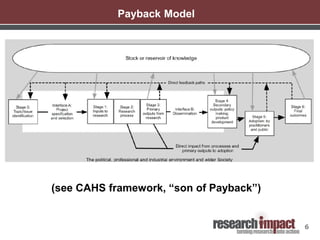
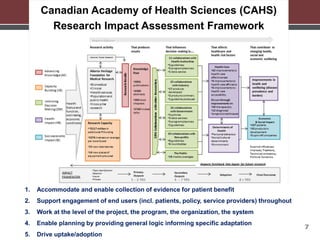
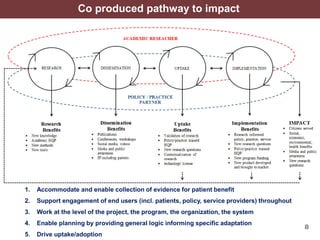
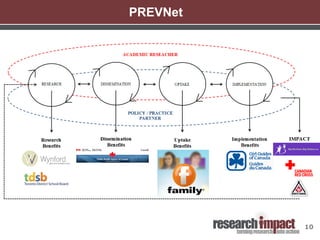
The document discusses various impact models and frameworks for assessing the impact of health research. It outlines criteria that effective impact models should meet, such as accommodating evidence collection for patient benefit, supporting engagement of end users throughout the research process, and enabling planning while allowing for specific adaptation. Several impact models and frameworks are described briefly, including the Knowledge to Action Cycle, Payback Model, Canadian Academy of Health Sciences Research Impact Assessment Framework, and co-produced pathway to impact model. The document advocates that impact planning must be tailored to each specific case while using generic frameworks as a starting point.