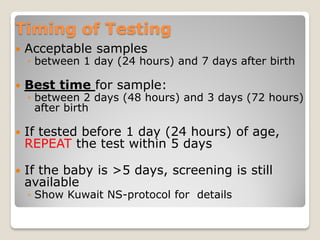
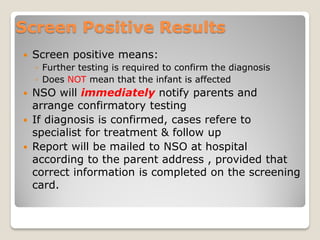
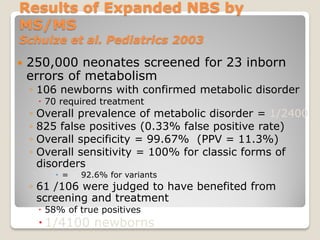
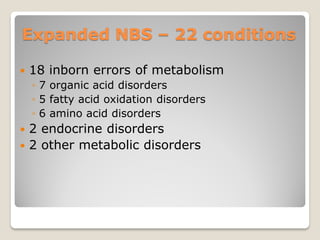
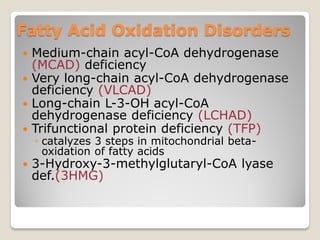
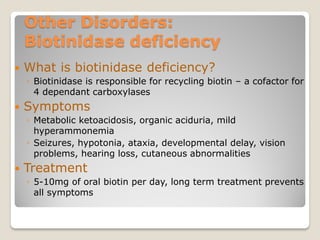
Kuwait has expanded its newborn screening program to screen for 22 primary disorders including 18 inborn errors of metabolism, 2 endocrine disorders, and 2 other metabolic disorders. The expanded screening provides benefits like early identification and intervention to reduce morbidity and mortality. Screening is done through heel prick samples that are tested at the Newborn Screening laboratory. Positive results require confirmatory testing while negative results are sent to hospitals. The expanded screening aims to improve outcomes for treatable genetic disorders.