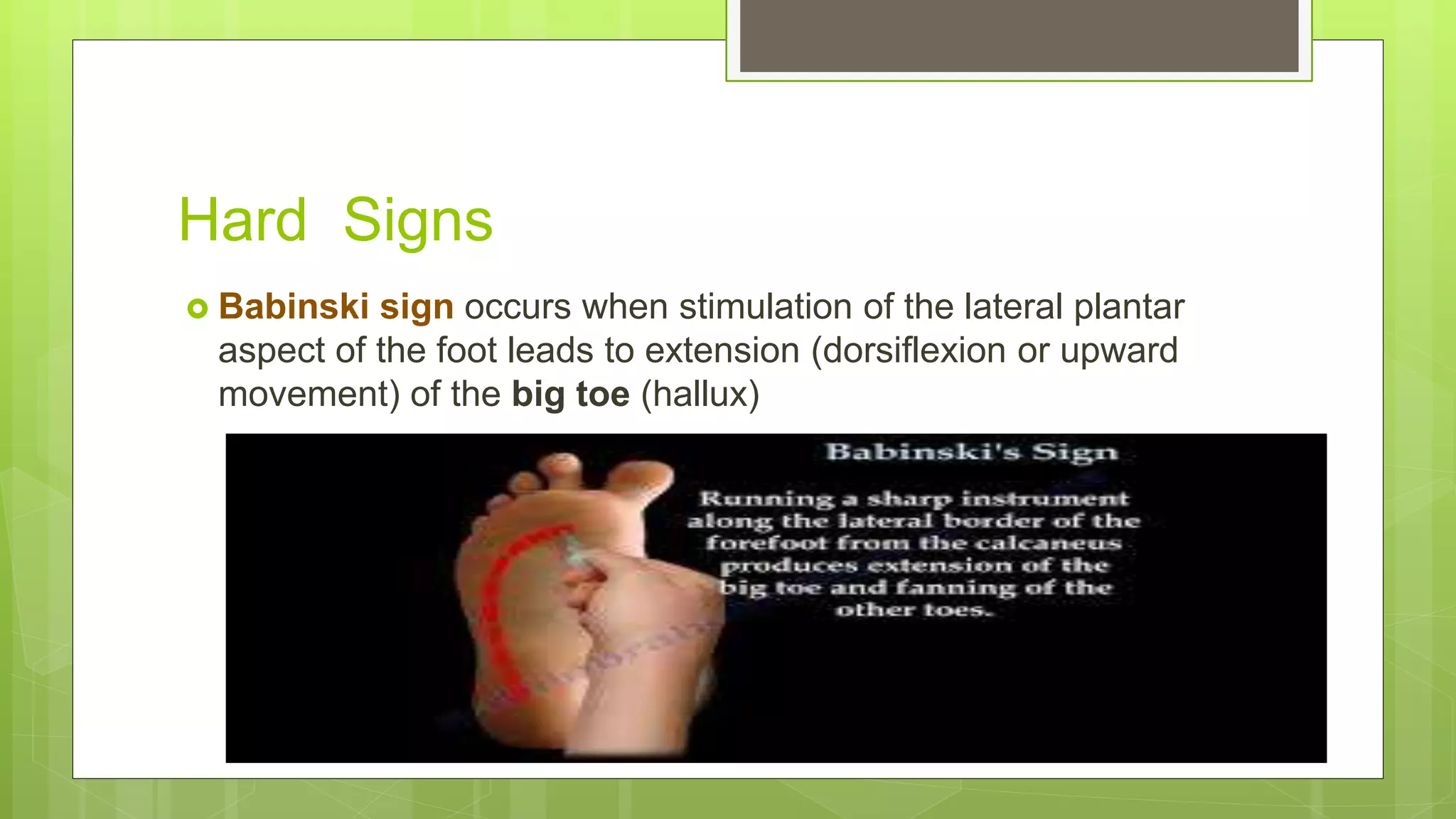
This document provides guidance on performing neurological examinations to evaluate patients. It describes how to examine cranial nerves, motor and sensory functions, reflexes, eye movements, smell, abnormal movements, and other signs. It emphasizes the importance of distinguishing between "hard" focal neurological signs and more subtle "soft" signs. Additional tests discussed include brain imaging, EEG, CSF analysis, sleep studies, and scales to evaluate disorders of consciousness. The goal is to localize neurological lesions and identify potential causes of psychiatric or cognitive symptoms.





















![Positron emission tomography (PET)
Metabolic assessment of the brain
Single- photon emission computed tomography (SPECT) metabolism of
brain, based on observations of regional differences in blood flow
Ioflupane (iodine- 123) injection for DaT Scan, a contrast agent to be
used with SPECT, can be used for detecting dopamine transporters
(DaT) in suspected idiopathic PD
Emerging imaging modalities,
including PET with amyloid tracers (e.g. Amyvid), sodium scans,
large- scale intrinsic network analysis via functional MRI [default
mode network (DMN), salience, etc.] are on the horizon as potentially
useful clinical tools to help disentangle the aetiology of neuropsychiatric
Symptoms](https://image.slidesharecdn.com/neurological-210126123010/75/Neurological-exam-oxford-bidaki-99-6-bahman-28-2048.jpg)


![Trauma Scales
Whereas a full interview
and the scales named earlier are appropriate in an awake, alert
patient without severe cognitive impairment, patients recovering
from severe TBI who are still in VS, MCS, or PTA/ PTCS will require
a tailored examination and different scales for assessment
[i.e.
the Coma Recovery Scale (CRS) for patients in VS and MCS
Orientation Log (O- Log)
Galveston Orientation and Amnesia
Test (GOAT)
CAP for patients in PTA/ PTCS]](https://image.slidesharecdn.com/neurological-210126123010/75/Neurological-exam-oxford-bidaki-99-6-bahman-34-2048.jpg)