This document provides information on bipolar disorder including:
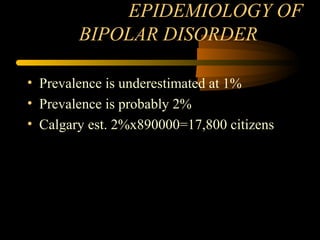
- The prevalence of bipolar disorder is estimated to be around 2% of the population, or about 17,800 people in Calgary.
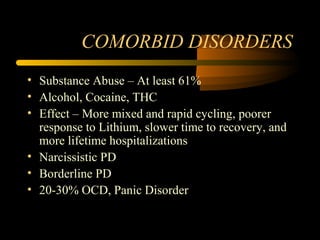
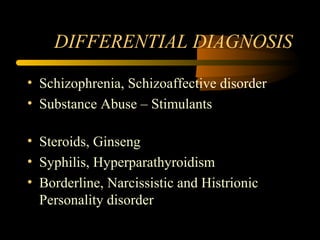
- Common comorbid disorders include substance abuse issues (61% of people with bipolar disorder), anxiety disorders, narcissistic or borderline personality disorders.
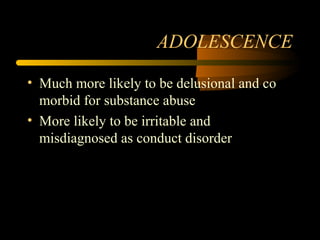
- Adolescents presenting with bipolar disorder are more likely to experience delusions or be misdiagnosed with conduct disorder due to irritability.
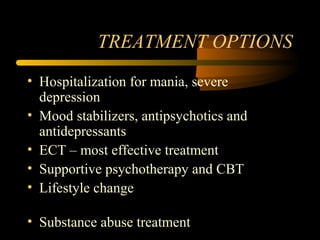
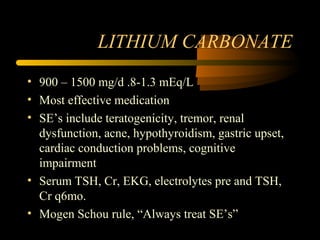
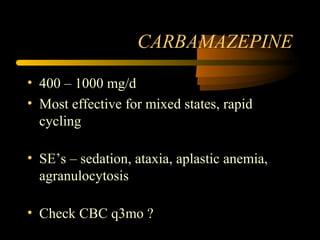
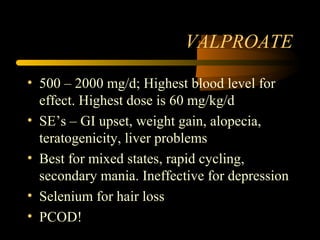
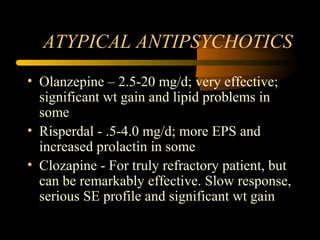
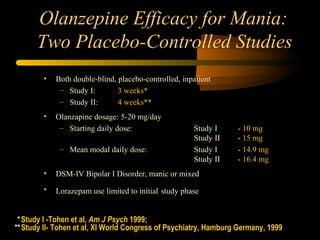
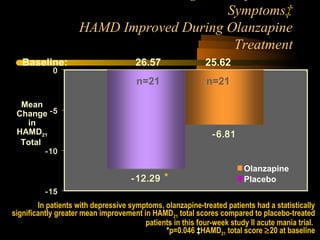
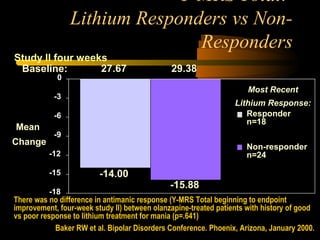
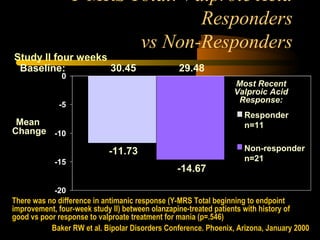
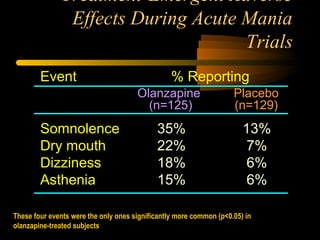
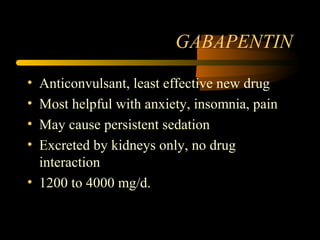
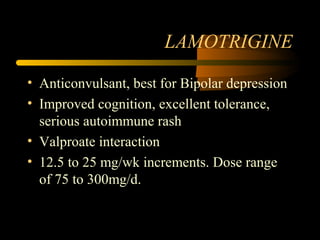
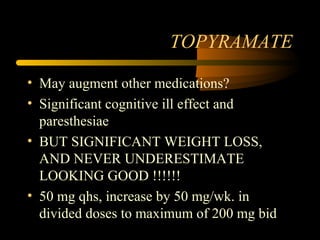
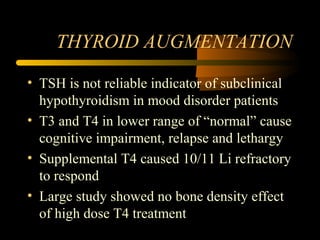
- Treatments discussed include mood stabilizers like lithium, lamotrigine, valproate, atypical antipsychotics like olanzapine, and augmentation with thyroid hormone or anticonv