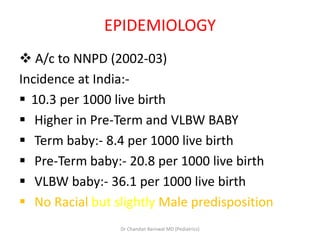
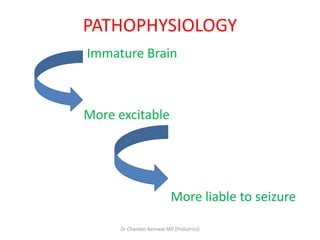
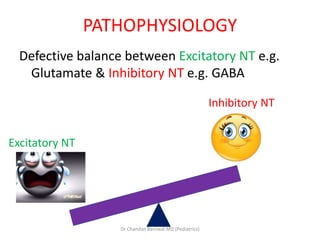
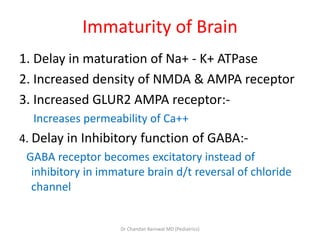
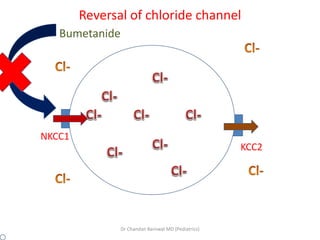
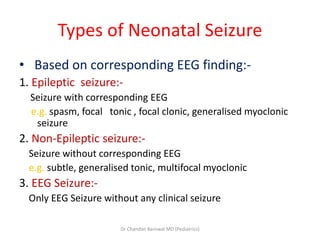
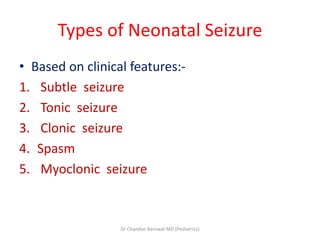
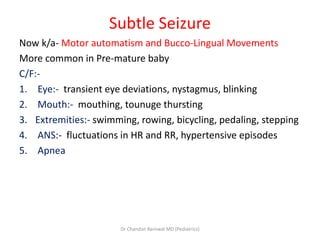
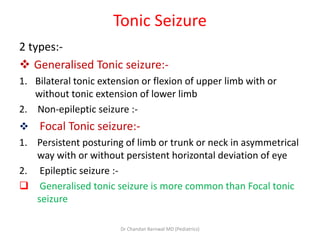
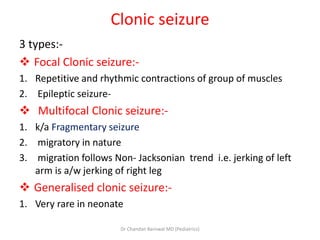
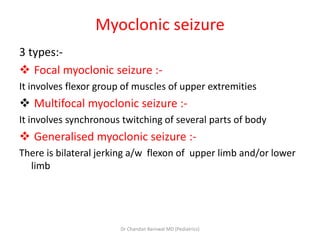
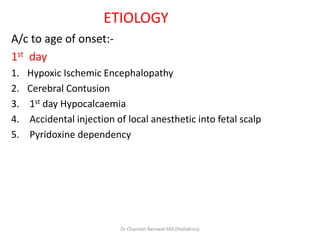
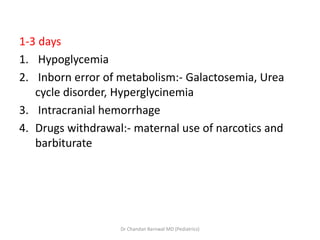
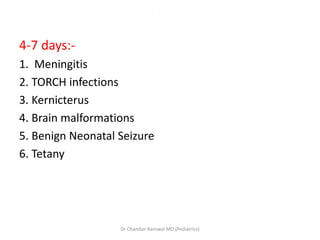
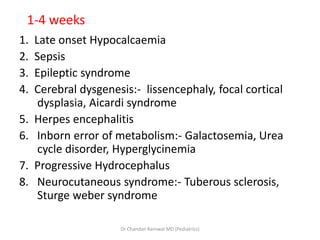
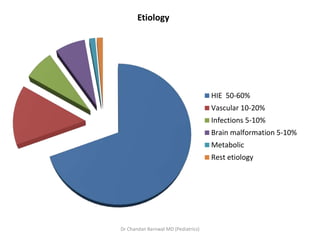
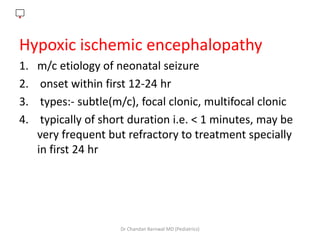
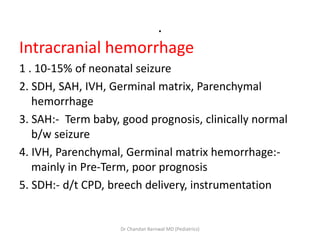
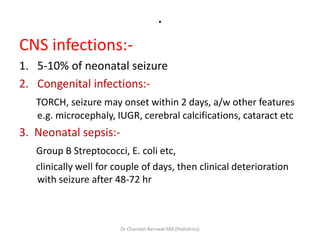
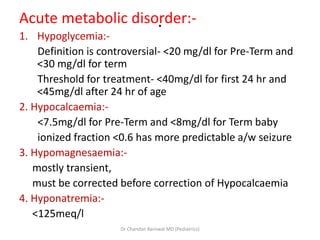
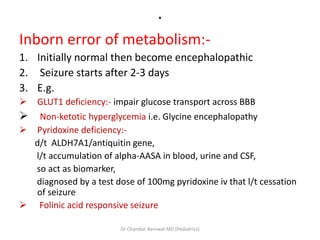
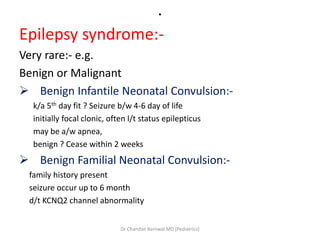
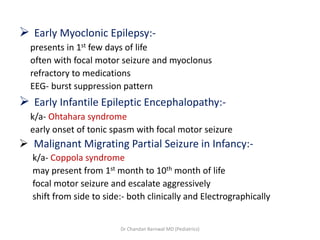
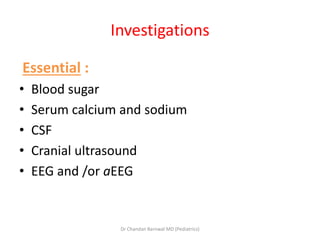
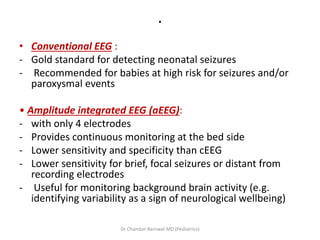
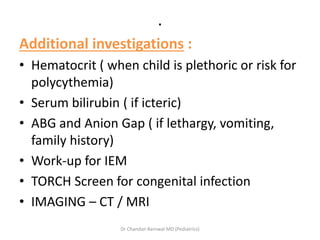
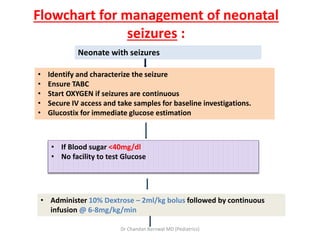
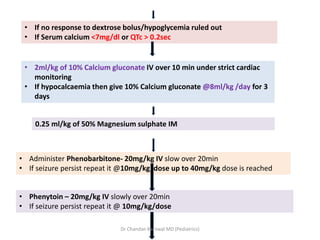
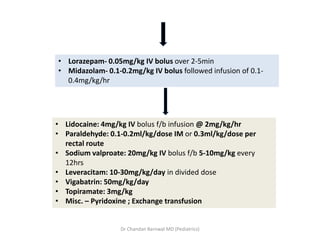
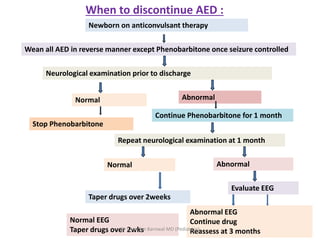
This document discusses neonatal seizures. It begins by defining seizures and noting that they are not uncommon in neonates and often indicate an underlying neurological condition. It then reviews epidemiological data on seizure incidence. The main causes of neonatal seizures are identified as hypoxic ischemic encephalopathy, intracranial hemorrhage, infections, metabolic disorders, and genetic conditions. The document outlines the various clinical presentations and classifications of neonatal seizures and diagnostic workup. Treatment involves identifying and treating the underlying etiology, maintaining glucose and electrolyte levels, and administering anti-seizure medications like phenobarbital. Careful monitoring is needed to determine when anti-seizure drugs can be safely discontinued.