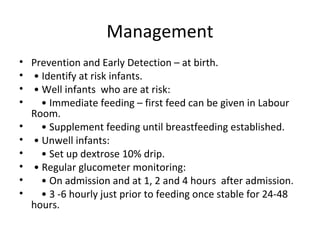
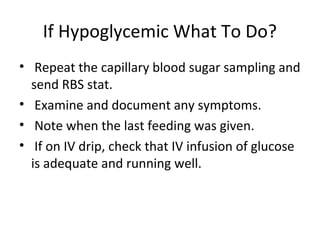
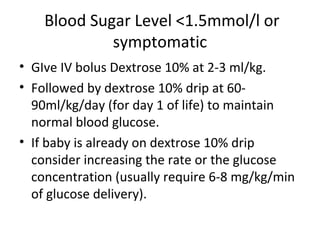
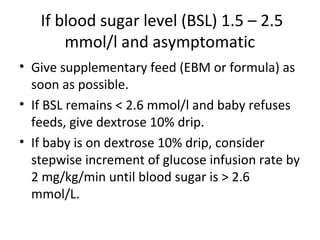
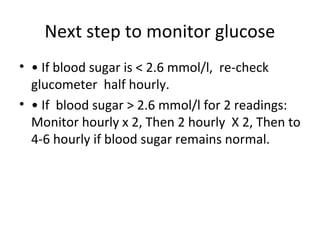
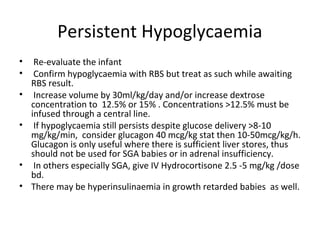
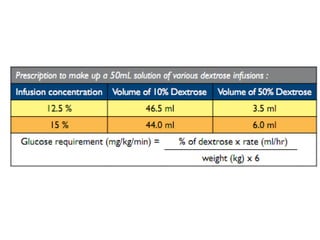
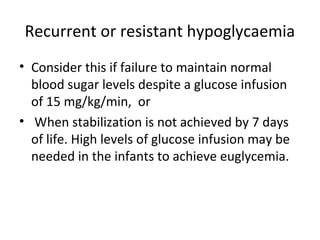
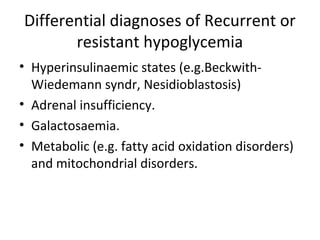
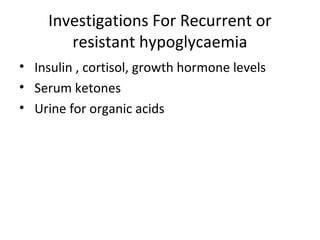
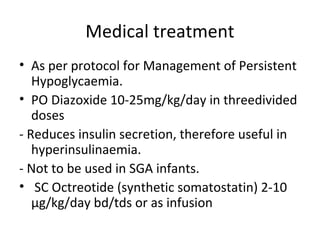
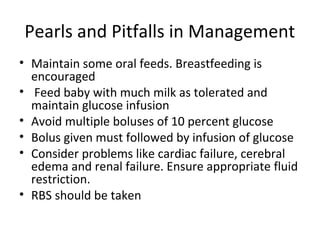
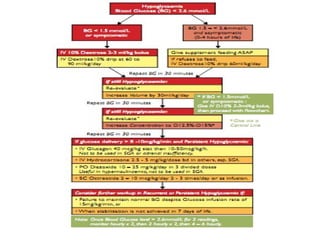
Neonatal hypoglycemia can occur in high-risk infants such as those born to diabetic mothers or who are preterm/small for gestational age. Symptoms may include jitteriness, apnea, or seizures. Management involves early feeding and glucose monitoring to prevent and detect hypoglycemia. For levels under 1.5 mmol/L, IV dextrose is given with frequent monitoring until levels rise above 2.6 mmol/L. Persistent hypoglycemia may require increased dextrose concentration or addition of medications like glucagon or hydrocortisone. Recurrent hypoglycemia suggests underlying conditions like hyperinsulinemia which require additional investigation and treatment with drugs to reduce insulin secretion.