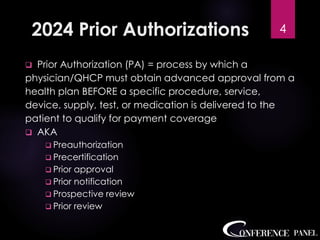
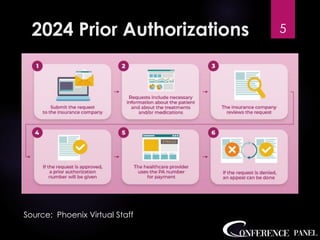
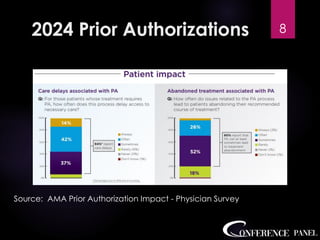
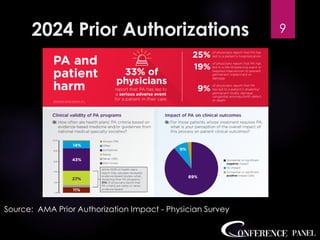
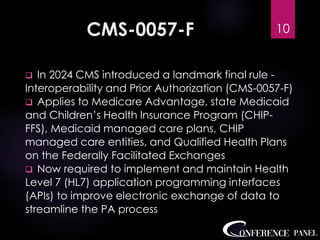
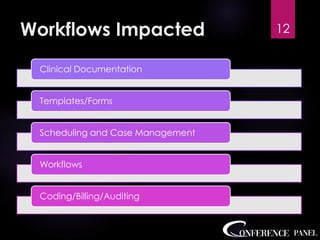
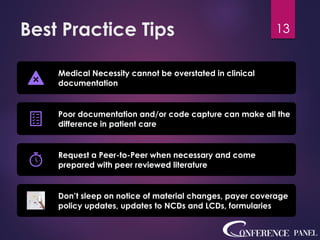
The document outlines the 2024 prior authorization process for medical providers, highlighting key challenges and regulatory changes, including a new CMS rule aimed at improving data exchange. It emphasizes the importance of medical necessity in determining care, noting the disconnect between insurance payers and healthcare providers. Additionally, it discusses the impact on various roles and workflows in the healthcare system.