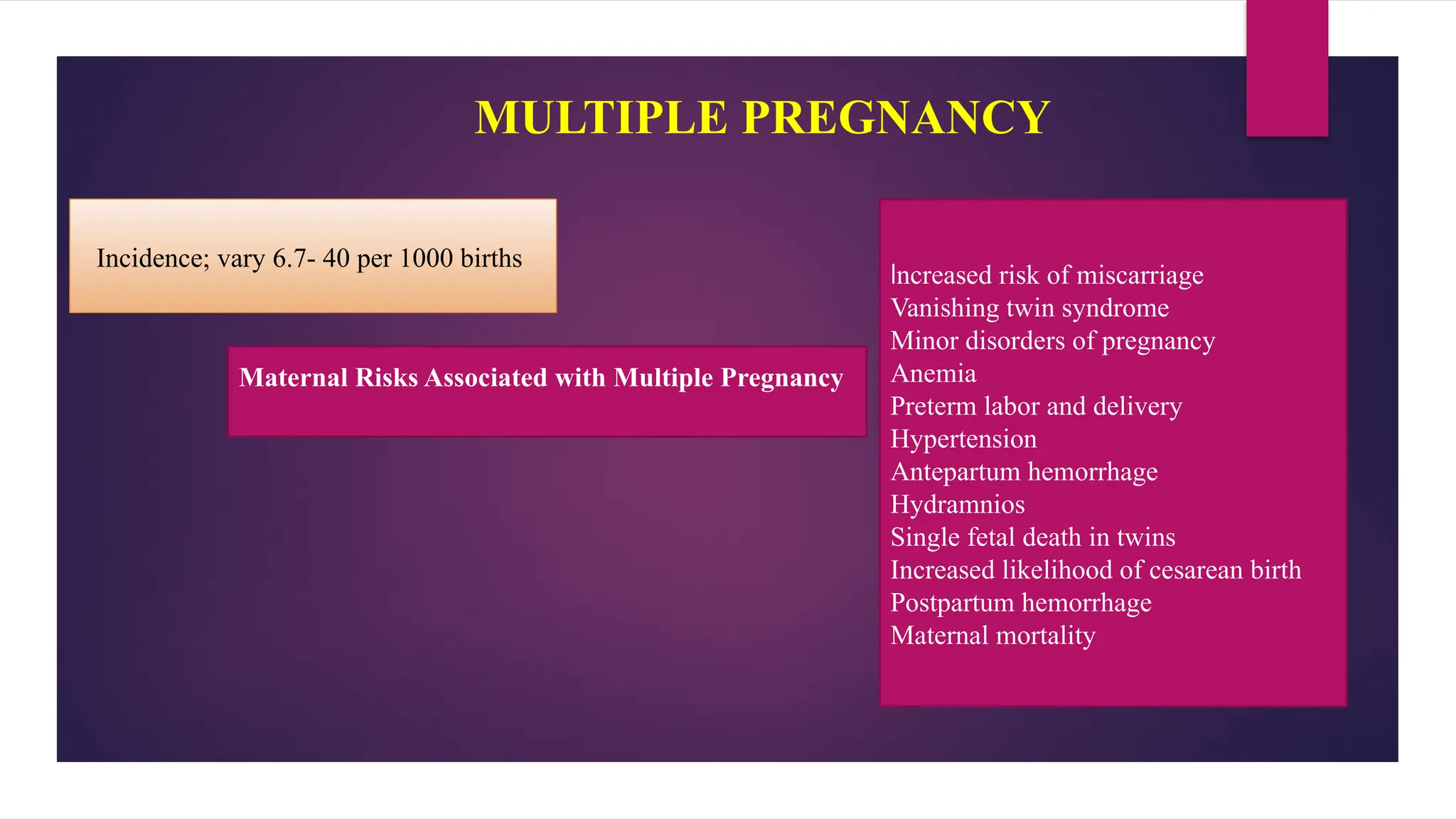
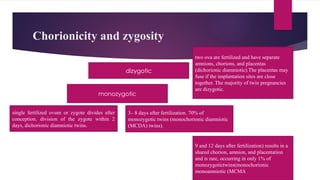
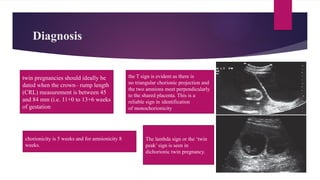
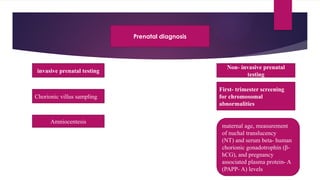
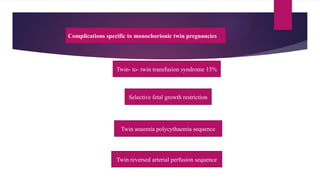
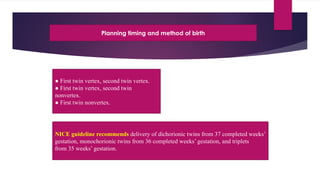
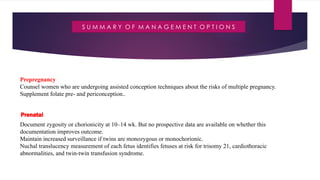
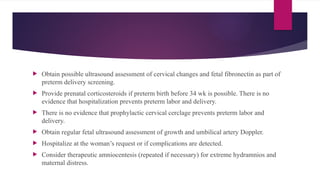
The document addresses the various risks and management strategies associated with multiple pregnancies, including miscarriage, preterm labor, and congenital anomalies. It differentiates between dizygotic and monozygotic twins, discusses prenatal screening methods, and outlines guidelines for delivery timing and management options. Key recommendations include increased surveillance for monochorionic twins and specific delivery protocols based on fetal positions.