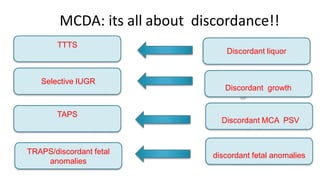
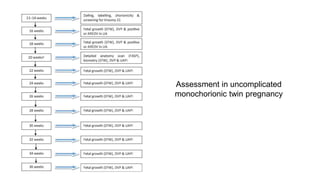
Multiple pregnancies can involve twins, triplets or more. Monitoring of monochorionic twins is important due to risks of twin-twin transfusion syndrome (TTTS), twin anemia-polycythemia sequence (TAPS), twin reversed arterial perfusion (TRAP) sequence, and selective growth restriction (sGR). TTTS occurs in 10-15% of monochorionic twins due to uneven blood flow through connecting blood vessels and can be diagnosed and treated with laser ablation. SGR can occur without fluid imbalance and is detected by significant fetal growth differences and abnormal Doppler readings of the umbilical artery. Close ultrasound monitoring every 2 weeks from 16 weeks is recommended for monochorionic twins.













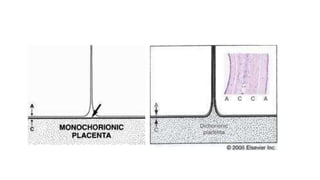
![Differences in chorionicity with single placenta
D / D ( fused placenta )
• Monozygotic or dizygotic
• Thick dividing membrane
> 2mm
• Twin peak / lambda sign
M / D
• Monozygotic
• Thin dividing membrane
2mm or less
• T sign
Chorionicity should be determined at the time the twin pregnancy is detected by
ultrasound based upon the number of placental masses, the appearance of the membrane
attachment to the placenta and the membrane thickness. This scan is best performed
before 14 weeks of gestation.[New 2016] (B)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-18-320.jpg)



![On ultrasound, the fetuses in twin pregnancies should be assigned
nomenclature (i.e. upper andlower, or left and right) and this should be clearly
documented in the woman’s case notes to ensureconsistency throughout
pregnancy. [New 2016] (C)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-22-320.jpg)

![Aneuploidy Screening in 1st T
Nuchal transluscency and maternal age.
Using the average NT:
NT in conjunction with maternal age: 75% sensitivity
Useful in the early detection or prediction of TTTS.
An NT threshold at the 95th percentile had a
PPV:43%
NPV: 91%
Women with monochorionic twins who wish to have aneuploidy screening should be offered
nuchal translucency measurements in conjunction with first trimester serum markers
(combined screening test) at 11+0 weeks to 13+6 weeks of gestation (crown–rump length 45–
84 mm). [New 2016] (C)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-26-320.jpg)
![Aneuploidy Screening in the 2nd T
Soft markers of Down syndrome
Nonossified nasal bone
linear arrangement of the tricuspid and mitral valves within the heart
thickened nuchal skin fold
slightly short humerus relative to head size
slightly short femur relative to head size
echogenic intracardiac focus
fetal hydronephrosis
In women with monochorionic twin pregnancies who ‘miss’ or who have unsuccessful first
trimester screening for aneuploidy, second trimester screening by the quadruple test should be
offered. [New 2016] (D)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-27-320.jpg)








![RCOG recommendation
• Fetal ultrasound assessment should take place every 2 weeks in uncomplicated
monochorionic pregnancies from 16+0 weeks onwards until delivery (D)
• At every ultrasound examination, liquor volume in each of the amniotic sacs should be
assessed and a deepest vertical pocket (DVP) depth measured and recorded, as well as the
umbilical artery pulsatility index (UAPI). Fetal bladders should also be visualised. (Appendix
III). [New 2016] (GPP)
• From 16+0 weeks of gestation, fetal biometry should be used to calculate an estimated fetal
weight (EFW) and the difference in EFW calculated and documented. As the risk of selective
growth restriction (sGR) extends to delivery, this should be performed at 2-weekly intervals
until delivery. [New 2016] (D)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-37-320.jpg)













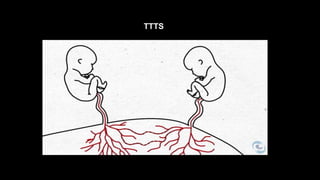
![• 95% monochorionic placentas have these but only 10-
15% suffer adverse outcomes
• TTTS and TRAP are the most well recognised
complications
• Suggested aetiology: deep anastomoses within
placental mass are usually btwn arteries and veins
which allow unidirectional blood flow
Screening for TTTS by first trimester nuchal translucency measurements should not be offered.
[New 2016] (C)
Screening for TTTS should be by ultrasound examination from 16+0 weeks onwards, at 2-weekly
intervals, noting and recording fetal biometry and liquor volumes (DVP). Fetal bladders should
also be visualised.](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-52-320.jpg)






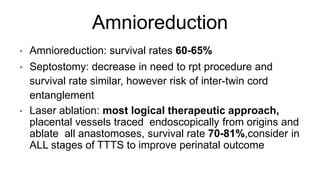
![Recommendation (RCOG)
Severe TTTS presenting < 26 weeks should be treated by laser
ablation rather than amnioreduction or septostomy Little
information about maternal morbidity after laser (A)
Delivery of monochorionic twin pregnancies previously complicated
by TTTS and treated should be between 34+0 and 36+6 weeks of
gestation. [New 2016] (D)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-62-320.jpg)





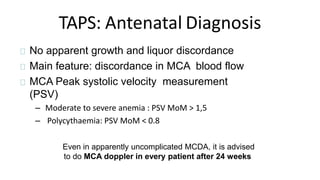
![Presence of arterial-arterial anastomoses is protective against TTTS
In TAPS: either less A-V anastomoses or more A-A
anastomoses
TAPS should be screened for following fetoscopic laser ablation for TTTS and in
other complicated monochorionic pregnancies requiring referral to a fetal medicine
centre (such as those complicated by sGR) by serial middle cerebral artery peak
systolic velocity (MCA PSV). [New 2016] (GPP)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-68-320.jpg)






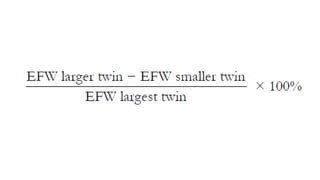
![Discordant Growth*
• Abdominal Circumference difference >20 mm
• EFW difference > 20%** (Larger twin as a reference)
• BPD > 6 mm
• FL > 6 mm
* Usually accompanied with abnormal UA doppler
** Latest evidence suggests that difference by 18% is significant
At each scan from 20 weeks of gestation (at 2-weekly intervals) onwards, calculate EFW discordance
using two or more biometric parameters. Calculate percentage EFW discordance using the following
formula: ([larger twin EFW – smaller twin EFW]/larger twin EFW) x 100. Liquor volumes as DVP should
be measured and recorded (to differentiate from TTTS). [New 2016] (C)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-77-320.jpg)
![Umbilical artery Doppler evaluation in monochorionic twins with sGR allows definition of prognosis and
potential morbidity. In particular, those with absent or reversed end-diastolic velocities (AREDV) and
‘cyclical’ umbilical artery Doppler waveforms (intermittent AREDV) are at increased risk of perinatal
mortality and morbidity (Appendix IV). [New 2016] (C)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-78-320.jpg)
![In type I sGR, planned delivery should be considered by 34–36 weeks of
gestation if there is satisfactory fetal growth velocity and normal umbilical
artery Doppler waveforms. [New 2016] (GPP)
In type II and III sGR, delivery should be planned by 32 weeks of gestation,
unless fetal growth velocity is significantly abnormal or there is worsening of
the fetal Doppler assessment. [New 2016] (GPP)
Abnormal ductus venosus Doppler waveforms (reversed flow during
atrial contraction) or computerised cardiotocography short-term
variation should trigger consideration of delivery. [New 2016]](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-79-320.jpg)
![Why is MCDAdifferent compared to DCDA?
• Death in one twin may lead to death of the other twin
• Neurological sequelae in surviving twin
Importance of close monitoring and timely decision for delivery!!!
• try to achieve good survival of both fetuses
• at least survival of one fetus with minimal neurological sequelae
In cases of early-onset sGR in association with poor fetal growth
velocity and abnormal umbilical artery Doppler assessments,
selective reduction may be considered an option. [New 2016] (C)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-80-320.jpg)

![Risks are not restricted to MC pregnancies with a prior diagnosis
of TTTS
Caused by acute haemodynamic changes around time of death, as
survivor haemorrhaging part of its circulating volume into the
circulation of the dying twin leading to hypotension and low
perfusion and eventually ischaemic end organ damage
After a single fetal death in a monochorionic pregnancy, clinicians should be
aware that the risks to the surviving twin of death or neurological abnormality
are of the order of 15% and 26%, respectively. [New 2016] (B)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-82-320.jpg)





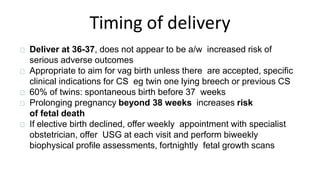

![Timing and mode of delivery in
uncomplicated monochorionic pregnancies
optimal timing and method of delivery for
otherwise uncomplicated monochorionic pregnancies
(without TTTS, sGR or TAPS)
Women with monochorionic twins should have timing of birth discussed and
be offered elective delivery from 36+0 weeks with the administration of
antenatal steroids, unless there is an indication to deliver earlier. [New 2016]
(C)
It is appropriate to aim for vaginal birth of monochorionic diamniotic
twins unless there are other specific clinical indications for caesarean
section.(A)](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-92-320.jpg)



![MCMA twins almost always have umbilical cord entanglement when
visualised using colour flow Doppler. Such a finding has not consistently
been demonstrated to contribute to overall morbidity and mortality. [New
2016] (D)
MCMA twins have a high risk of fetal death and should be delivered by
caesarean section between 32+0 and 34+0 weeks. [New 2016] (D)
specific problems of MCMA pregnancies and how should they
be managed](https://image.slidesharecdn.com/multiplepregnancylectureryan-180129195300/85/Multiple-pregnancy-lecture_r_yan-96-320.jpg)
