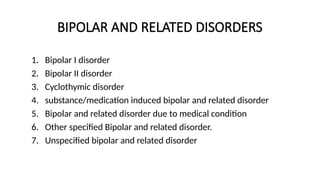
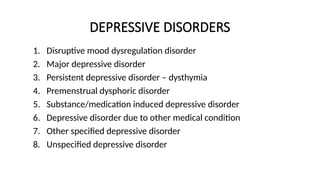
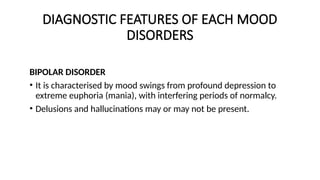
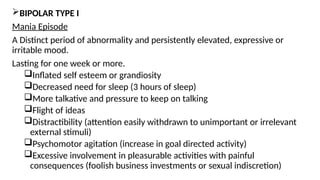
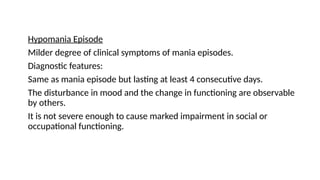
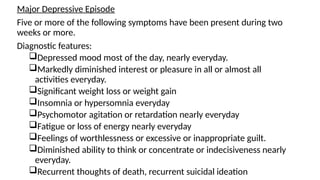
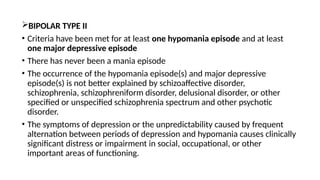
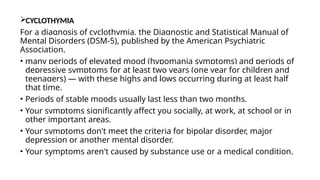
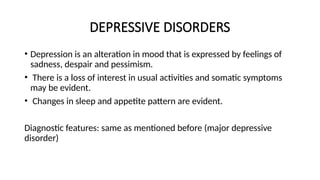
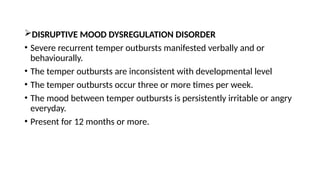
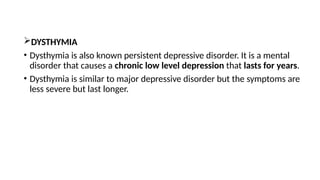
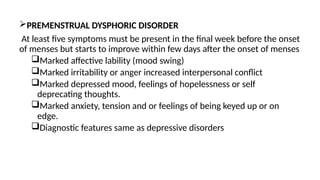
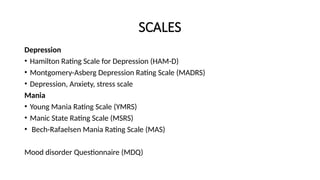
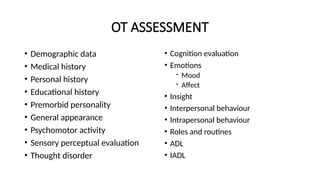
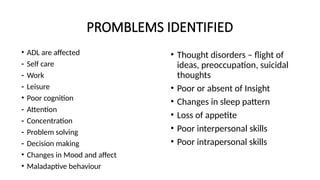
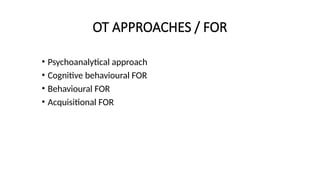
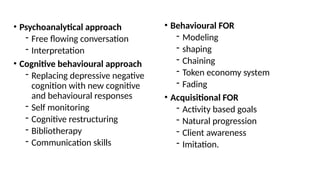
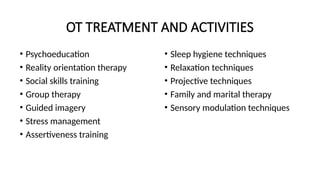
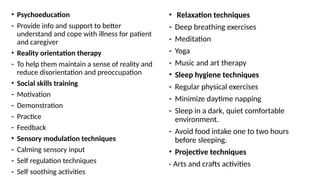
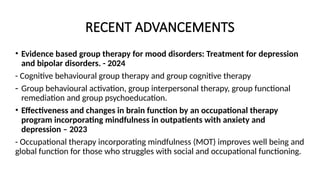
This document provides a comprehensive overview of mood disorders, focusing on their classification, diagnostic features, pathophysiology, causes, and medical management. It categorizes mood disorders as either bipolar or depressive and outlines specific disorders within these categories, detailing symptoms and treatment approaches, including occupational therapy interventions. Recent advancements in evidence-based group therapy and the impact of mindfulness on treatment outcomes are also highlighted.