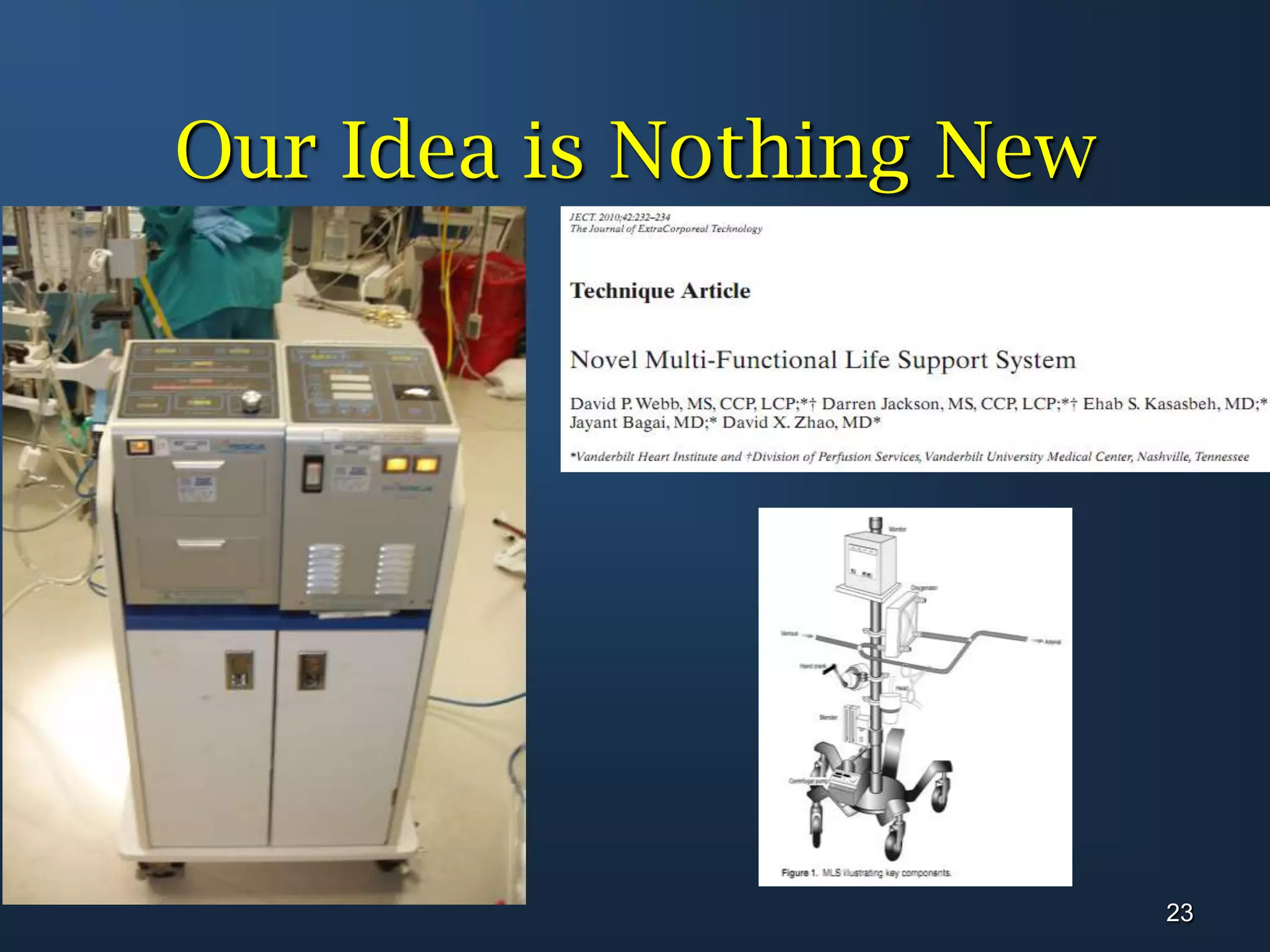
The document presents a case series of 3 patients who were successfully treated with a modernized extracorporeal life support (ECLS) system. Patient A was a 45-year-old woman who presented with viral myocarditis and reduced ejection fraction. She was placed on ECLS and Impella support and recovered. Patient B was a 62-year-old woman who arrested during a cardiac catheterization for an anterior MI. ECLS was initiated and she was discharged home after recovering. Patient C was a 20-year-old woman with post-partum cardiomyopathy and reduced EF who was also treated with ECLS and made a full recovery. The presentation concludes that modern ECLS systems have reduced challenges and should be readily