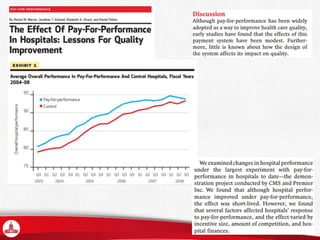
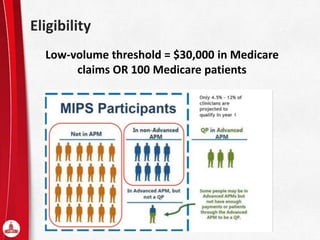
The document provides an overview of the MACRA framework, emphasizing the pay-for-performance (P4P) model which incentivizes clinicians to improve care quality and utilize health information technology. It outlines the components of the Merit-Based Incentive Payment System (MIPS), specific eligibility requirements, and performance categories while addressing the impact on various medical specialties and health equity. Future challenges include the consolidation of small practices and the need for quality improvement measures amidst increasing health disparities.